Researchers claim that after putting the Fmr1 gene into the brains of very young transgenic mice that had been genetically modified to lack this gene, they were able to alleviate Fragile X syndrome symptoms. When the researchers monitored brain activity for evidence of anxiety and hyperactivity in response to stimuli such as stresses and sounds, they discovered that reactivating the gene in these mice had resulted in them no longer exhibiting Fragile X syndrome symptoms.
Fragile X syndrome, or FXS, is a prominent hereditary cause of autism that affects around one in every 4,000 boys and one in every 6,000 girls. Increased anxiety, intellectual incapacity, repetitive behaviors, social communication problems, and poor sensory processing are some of the symptoms. People with FXS usually do not have the fragile X mental retardation 1 gene, or Fmr1, in their brain cells. If this gene is present in their cells, it is quiet and does not produce a protein known as FMRP.
Researchers from the University of California, Riverside, report in the journal Neurobiology of Disease that by injecting Fmr1 into the brains of very young transgenic mice that had been genetically modified to lack this gene, they were able to alleviate FXS symptoms. When the researchers monitored brain activity for evidence of anxiety and hyperactivity in response to stimuli such as stresses and sounds, they discovered that reactivating the Fmr1 gene in these mice had resulted in them no longer exhibiting FXS symptoms.
In the current study, we inserted the Fmr1 gene into excitatory neurons in the second and third postnatal weeks of mice. Our research shows that it is not too late to manipulate the brain during this time period. We chose these neurons because they establish control over inhibitory neurons that are dysfunctional in FXS.
Professor Iryna M. Ethell
“Our findings suggest that reactivating the Fmr1 gene has favorable consequences,” said Iryna M. Ethell, a professor of biomedical sciences at the University of California, Riverside School of Medicine, who led the study.
Ethell’s laboratory, in partnership with Khaleel A. Razak, a psychology professor, chose very young mice (less than 3 weeks old) for their investigation because brains are most changeable early in life; the equivalent in humans is around the first 3-5 years.
“For humans, the first 3-5 years are critical in brain development,” Ethell said. “It’s important, therefore, that this early period be targeted in FXS.”
Excitatory and inhibitory neurons exist in the mouse brain, just as they do in the human brain. In contrast to excitatory neurons, which cause information to go forward, inhibitory neurons operate as a brake, limiting superfluous activity and adjusting brain activity to specific signals.
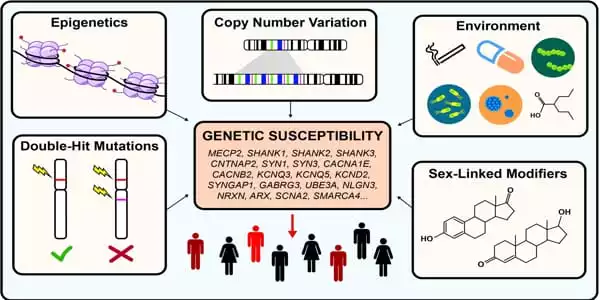
Ethell and two colleagues recently published a review article in Nature Neuroscience demonstrating that inhibitory neuron dysfunction is a frequent pathology in hereditary diseases associated with autistic spectrum disorders, or ASD.
“In the current study, we inserted the Fmr1 gene into excitatory neurons in the second and third postnatal weeks of mice,” Ethell explained. “Our research shows that it is not too late to manipulate the brain during this time period. We chose these neurons because they establish control over inhibitory neurons that are dysfunctional in FXS. We do not know if our strategy would be beneficial in adults at this time. That research would be a natural progression in this line of work.”
The manner in which Ethell and her colleagues introduced the Fmr1 gene into the mouse brain differs from the manner in which the gene could potentially be introduced into the human brain. However, the end result would be the same, according to Ethell. CRISPR, a potent technique for modifying genomes, would most likely be employed to reactivate Fmr1 in the human brain, according to her.
“FXS is typically identified early in a person’s life,” she explained. “We cannot emphasize enough that the early years are ideal for reactivating the Fmr1 gene. It gives hope that even if a child lacks this gene, it can still be introduced, allowing the child to live a normal life free of FXS. As gene reactivation for the treatment of FXS gains popularity, our findings show that Fmr1 re-expression may be beneficial during the early period of brain plasticity in mice, which roughly corresponds to the first three years of human life, when ASD symptoms initially appear in infancy.”
Following that, the research team will work to reestablish function in the adult FXS brain.
“The main difficulty is that the adult brain is not as plastic,” Ethell explained. “Young minds are capable of almost anything. However, as an adult, have you attempted to learn a new language?”
The National Institutes of Health, the Department of Defense, and the FRAXA Research Foundation all contributed to the study. The National Institute of Neurologic Disorders and Stroke also supported first author Maham Rais with a National Research Service Award Fellowship.