According to UConn Health experts, removing aged, defective cells from human fat reduces diabetic symptoms. The breakthrough could pave the way for novel treatments for Type 2 diabetes and other metabolic illnesses.
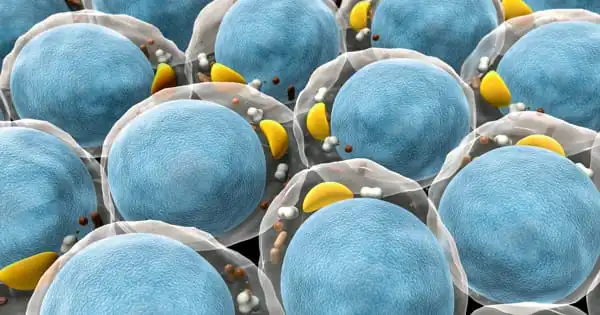
Your body’s cells are constantly renewing themselves, with older cells aging and dying while new ones are formed. But, every now and then, that process goes astray. Damaged cells can sometimes be found. They are known as senescent cells because they linger and have a negative impact on the cells around them. Their negative influence alters how nearby cells manage glucose or proteins, resulting in metabolic issues.
Researchers from UConn Health and the Mayo Clinic discovered that removing senescent cells from adipose tissue reduces insulin resistance in obese rats. Importantly, eliminating these senescent cells from human adipose tissue, which have high activity in the levels of a gene called p21, reduces insulin resistance when transplanted into mice. These findings establish the groundwork for using senescent cells as a potential therapeutic to treat insulin resistance and slow the progression of type 2 diabetes.
We investigated the effectiveness of a combination of investigational medicines, dasatinib and quercetin. Dasatinib and quercetin have previously been found to increase longevity and improve health in elderly mice.
Ming Xu
Diabetes type 2 is the most common metabolic condition in the United States. According to the Centers for Disease Control and Prevention, it affects around 34 million people, or one out of every ten Americans (CDC). The majority of diabetics have insulin resistance, which is linked to obesity, a lack of exercise, and a poor diet. However, it also has a lot to do with senescent cells in people’s body fat, according to new research by Ming Xu and colleagues at UConn Health School of Medicine. And removing those senescent cells appears to reduce diabetic behavior in obese mice, the researchers report in Cell Metabolism.
Ming Xu, assistant professor at the UConn Center on Aging and the Department of Genetics and Genome Sciences at UConn Health, led the study, with substantial contributions from UConn Health researchers Lichao Wang and Binsheng Wang. According to the researchers, alleviating the harmful effects of fat on metabolism was a remarkable result. If therapy worked that well in humans, it would be a game-changer for diabetes treatment.
Xu and colleagues investigated the effectiveness of a combination of investigational medicines, dasatinib, and quercetin. Dasatinib and quercetin have previously been found to increase longevity and improve health in elderly mice. They discovered that these medicines can kill senescent cells from human fat tissue cultures in their investigation. Individuals with obesity who were known to have metabolic issues gave the tissue. Without therapy, human fat tissues caused metabolic difficulties in immune-compromised mice. The negative effects of adipose tissue were nearly completely eradicated after therapy with dasatinib and quercetin.

“These medications have the potential to make human fat healthier,” adds Xu. “The results were really impressive, and they paved the way for future clinical trials.”
Xu and his colleagues at UConn Health and the Mayo Clinic are currently exploring clinical trials with the dasatinib and quercetin combo to investigate if the medications may improve Type 2 diabetes in humans. “Although these preclinical results were very promising,” Xu stressed, “large scale clinical trials are absolutely important to investigate the efficacy and safety of these medications in humans before clinical usage.”
The researchers are also looking into a previously unknown senescent cell population. These senescent cells have high amounts of p21, a cyclin-dependent kinase inhibitor that is also a crucial marker for cellular senescence. Xu’s team found that clearing these senescent cells once a month is helpful for both reducing the development of diabetes and easing existing diabetic symptoms in obese mice utilizing a newly designed mouse model. According to Xu, earlier study has concentrated on different cell markers, but the effects of clearing away cells primarily expressing p21 on easing diabetes were so significant that this marker should receive greater attention.
“While these preclinical results were very promising,” Dr. Xu says, “large-scale clinical trials are absolutely important to investigate the efficacy and safety of these medications in humans before clinical usage.” Furthermore, the human adipose tissue transplantation model created here can be used to test a variety of senolytic medicines or other agents on human fat tissues to treat insulin resistance, which has the potential to be a valuable tool for future precision medicine.