A tiny gadget developed by MIT scientists and the Singapore-MIT Alliance for Research and Technology could increase the safety and efficacy of cell therapy treatments for patients with spinal cord injury.
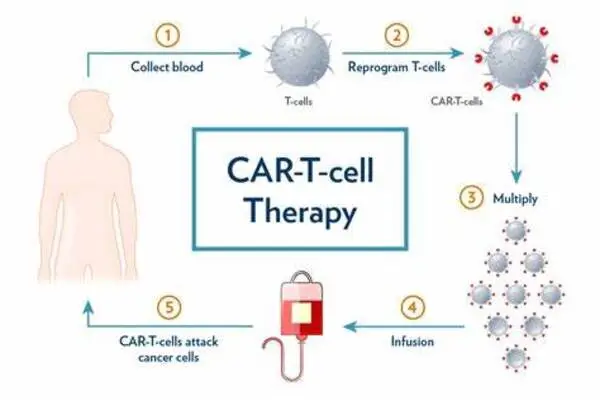
In cell therapy, clinicians alter some skin or blood cells from a patient to produce induced pluripotent stem cells (iPSCs). To cure a spinal cord injury, they would coax these pluripotent stem cells into progenitor cells, which will develop into spinal cord cells. These progenitor cells are subsequently put back into the patient.
These new cells are capable of regenerating a portion of the wounded spinal cord. However, pluripotent stem cells that do not fully differentiate into progenitors might develop malignancies. This study team created a microfluidic cell sorter that can remove almost half of the undifferentiated cells (those that could become cancers) in a batch while causing no damage to the fully established progenitor cells.
Spinal cord progenitor cells derived from pluripotent stem cells hold great promise, since they can generate all cell types found within the spinal cord to restore tissue structure and function. To be able to effectively utilize these cells, the first step would be to ensure their safety, which is the aim of our work.
Jongyoon Han
The high-throughput system, which does not require any special chemicals, has a sorting capacity of over 3 million cells per minute. Furthermore, the researchers demonstrated that connecting many devices can sort more than 500 million cells per minute, making it a more practical option for improving the safety of cell therapy treatments in the future.
Plus, the plastic chip that contains the microfluidic cell sorter can be mass-produced in a factory at very low cost, so the device would be easier to implement at scale.
“Even if you have a life-saving cell therapy that is doing wonders for patients, if you cannot manufacture it cost-effectively, reliably, and safely, then its impact might be limited. Our team is passionate about that problem — we want to make these therapies more reliable and easily accessible,” says Jongyoon Han, an MIT professor of electrical engineering and computer science and of biological engineering, a member of the Research Laboratory of Electronics (RLE), and co-lead principal investigator of the CAMP (Critical Analytics for Manufacturing Personalized Medicine) research group at the Singapore-MIT Alliance for Research and Technology (SMART).
Reducing risk
The cancer risk posed by undifferentiated induced pluripotent stem cells remains one of the most pressing challenges in this type of cell therapy. “Even if you have a very small population of cells that are not fully differentiated, they could still turn into cancer-like cells,” Han adds.
Clinicians and researchers often seek to identify and remove these cells by looking for certain markers on their surfaces, but so far researchers have not been able to find a marker that is specific to these undifferentiated cells. Other methods use chemicals to selectively destroy these cells, yet the chemical treatment techniques may be harmful to the differentiated cells.
The high-throughput microfluidic sorter, which can sort cells based on size, had been previously developed by the CAMP team after more than a decade of work. It has been previously used for sorting immune cells and mesenchymal stromal cells (another type of stem cell), and now the team is expanding its use to other stem cell types, such as induced pluripotent stem cells, Han says.
“We are interested in regenerative strategies to enhance tissue repair after spinal cord injuries, as these conditions lead to devasting functional impairment. Unfortunately, there is currently no effective regenerative treatment approach for spinal cord injuries,” Chew says. “Spinal cord progenitor cells derived from pluripotent stem cells hold great promise, since they can generate all cell types found within the spinal cord to restore tissue structure and function. To be able to effectively utilize these cells, the first step would be to ensure their safety, which is the aim of our work.”
The team discovered that pluripotent stem cells tend to be larger than the progenitors derived from them. It is hypothesized that before a pluripotent stem cell differentiates, its nucleus contains a large number of genes that haven’t been turned off, or suppressed. As it differentiates for a specific function, the cell suppresses many genes it will no longer need, significantly shrinking the nucleus.
The microfluidic device leverages this size difference to sort the cells.
Spiral sorting
Microfluidic channels in the quarter-sized plastic chip form an input, a spiral, and four exits that produce cells of varying sizes. As the cells are driven through the spiral at high speeds, they are subjected to a variety of forces, including centrifugal force. These forces work against each other to concentrate the cells in a specific area within the fluid stream. This concentrating point will vary depending on the size of the cells, effectively sifting them through various outlets.
The researchers discovered that running the sorter twice, first at a slower pace to allow larger cells to attach to the walls while smaller cells are sorted out, and then at a faster speed to sort out larger cells, improved its operation. In a sense, the device operates like a centrifuge, but the microfluidic sorter does not require human intervention to pick out sorted cells, Han adds.
The researchers showed that their device could remove about 50 percent of the larger cells with one pass. They conducted experiments to confirm that the larger cells they removed were, in fact, associated with higher tumor risk.
“While we cannot eradicate 100% of these cells, we believe this will considerably lower the risk. Hopefully, the initial cell type is good enough to prevent too many undifferentiated cells. “Then this process may make these cells even safer,” he argues.
Importantly, the low-cost microfluidic sorter, which can be built at scale using regular manufacturing procedures, does not require any filtration. Filters can become clogged or break down, therefore a device without filters can be utilized for considerably longer periods of time.
Now that they’ve demonstrated effectiveness on a small scale, researchers are moving on to larger experiments and animal models to see if the purified cells perform better in vivo. Nondifferentiated cells can become tumors, but they can have other random effects in the body, so removing more of these cells could boost the efficacy of cell therapies, as well as improve safety.