Type 1 diabetes is an autoimmune disease in which the immune system attacks and destroys the insulin-producing cells in the pancreas. Insulin is a hormone that regulates blood sugar levels, and without it, blood sugar levels can become dangerously high. Current treatments for Type 1 diabetes include insulin injections or pumps to regulate blood sugar levels, as well as monitoring and managing diet and exercise. There is ongoing research into potential cures and new treatments, including transplantation of insulin-producing cells and the use of immunotherapy to prevent the immune system from attacking these cells.
Using a new screening technique that involves tagging each biomaterial formulation in a library of hundreds with a unique ‘barcode,’ scientists identified three biomaterial formulations that could help develop a more sustainable, long-term, self-regulating way to treat Type 1 diabetes. Getting a host immune system to tolerate the presence of implanted insulin-secreting cells could be life-changing for the more than 700 million people worldwide who have Type 1 diabetes.
Omid Veiseh, a bioengineer at Rice University, and his colleagues discovered new biomaterial formulations that could help turn the page on Type 1 diabetes treatment, paving the way for a more sustainable, long-term, self-regulating approach to the disease. To accomplish this, they devised a new screening technique that involves assigning a unique “barcode” to each biomaterial formulation in a library of hundreds before implanting them in live subjects.
In Type 1 diabetes patients, the immune system attacks the pancreatic insulin-producing cells. As those cells die, the patient loses the ability to control their blood glucose.
Omid Veiseh
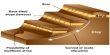
According to the study published in Nature Biomedical Engineering, encapsulating human insulin-secreting islet cells in one of the alginate formulations provided long-term blood sugar level control in diabetic mice. Catheters coated with two additional high-performance materials did not clog.
“This work was motivated by a major unmet need,” Veiseh, a Rice assistant professor of bioengineering and Cancer Prevention and Research Institute of Texas scholar, said. “In Type 1 diabetes patients, the immune system attacks the pancreatic insulin-producing cells. As those cells die, the patient loses the ability to control their blood glucose.”
For decades, scientists worked toward what Veiseh referred to as the “‘holy grail’ goal of housing islet cells inside a porous matrix made of a protective material that would allow the cells to access oxygen and nutrients without getting clobbered by the host’s immune system.” However, due in part to screening constraints, materials with optimal biocompatibility proved extremely difficult to find. On the one hand, the immune system response to a particular implanted biomaterial can only be evaluated in a live host.

“The problem is that the immune response needs to be investigated inside the body of these diabetic mice, not in a test tube,” said Boram Kim, a graduate student in the Veiseh lab and study co-lead author. “This means that in order to screen these hundreds of alginate molecules, you’ll need hundreds of animal test subjects. Our plan was to screen for hundreds of biomaterials in the same test subject at the same time.”
On the other hand, different biomaterial formulations appear identical, making it impossible to distinguish high-performing ones in the absence of a distinguishing feature. This made it impossible to test more than one biomaterial per host.
“They are different materials but they look the same,” Veiseh said. “And once they are implanted in the body of a test subject and then taken out again, we cannot distinguish between the materials and we would be unable to identify which material formulation worked best.”
To overcome these limitations, Veiseh and colleagues devised a method to label each alginate formulation with a unique ‘barcode,’ allowing them to identify the best performers. “We paired each modified biomaterial with human umbilical vein endothelial cells (HUVEC) from a different donor,” explained Kim.
“The HUVEC cells, because they come from unique donors, act as a barcode that allows us to tell what material was used initially,” Veiseh explained. “The ones with living cells are the ones who win.” When we found them, we sequenced their genomes to determine which material was paired with them. That’s how we found the biggest hits.”
Trials are underway for stem cell-derived islet cell use in diabetic patients. However, current islet treatments require immunosuppression, making it a taxing way to treat Type 1 diabetes.
“Currently, in order to use implanted islet cells in diabetic patients, you have to suppress the entire immune system, just as if you were trying to do an organ transplant,” Veiseh said. “That comes with a lot of complications for the patient. They can develop cancer, they can’t fight infections, so, for the vast majority of patients, it’s better to actually do the insulin therapy where they inject themselves. With this biomaterial-encapsulation strategy, no immunosuppression is needed.”
Placing live HUVEC cells inside biomaterial capsules increased the likelihood of the host immune system detecting a foreign presence. This strengthens the experiment over simply testing for immune response to biomaterials alone.
“We wanted to test a library of these materials, with the selection pressure of having cells inside the beads that makes it harder for the material not to get noticed by the immune system,” Veiseh explained. “There’s a lot of interest from all of the islet cell manufacturers in being able to get rid of immunosuppression and instead use these alginate hydrogel matrices to protect the implanted cells.”
With fewer live test subjects, the new high-throughput “barcoding” approach can be used to screen for other medical applications. “That actually feeds into a lot of other projects in my lab where we’re doing biologic production from cells for other disease indications,” said Veiseh.
“The same changes can be made to all types of materials that go into the body.” This is not restricted to cell transplantation. The technology we created can be combined with a wide range of device concepts. Some diabetic patients, for example, use automated pump systems to self-administer insulin. Because the catheters on those pump systems become clogged, they must be replaced every few days. We were able to demonstrate that coating catheters with these new materials kept them from clogging.”