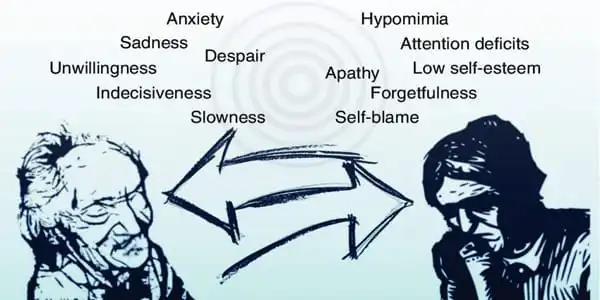
Early Alzheimer’s disease and depression have many symptoms, making it difficult to distinguish between the conditions – even for specialists. Furthermore, many persons with Alzheimer’s disease are also depressed. Therapy is vital for persons suffering from depression alone, but it is also critical for those suffering from Alzheimer’s disease and depression to receive treatment for their depression.
Alzheimer’s disease (AD), a neurological illness characterized by progressive dementia that affects over 6 million Americans, has long been associated to depression, according to epidemiological statistics. A recent study has identified shared genetic variables in both depression and Alzheimer’s disease. Importantly, the researchers discovered that depression played a causal role in the development of Alzheimer’s disease, and individuals with worse depression had a faster deterioration in memory. Elsevier publishes the study in Biological Psychiatry.
Aliza Wingo, MD, a co-senior author from Emory University School of Medicine in Atlanta, USA, stated of the discovery, “It raises the potential that there are genes involved in both diseases. While the shared genetic basis is minor, the data suggest that depression may have a causative role in dementia.”
The researchers used a genome-wide association study (GWAS), which examines the whole genome for areas of commonality associated with certain illnesses. The GWAS discovered 28 brain proteins and 75 transcripts (messages that encode proteins) that were linked to depression. Among them, 46 transcripts and 7 proteins were linked to Alzheimer’s disease symptoms. The findings point to a common genetic basis for the two diseases, which could explain the higher risk of AD associated with depression.
This study demonstrates a genetic link between depression and Alzheimer’s disease and related dementia. This is significant because it may explain, at least in part, the well-established epidemiologic link between depression and increased dementia risk.
Thomas Wingo
Although prior research have used GWAS to investigate AD and depression, the current study was strengthened by the use of bigger, newly available data sets that showed more precise information.
“This study demonstrates a genetic link between depression and Alzheimer’s disease and related dementia,” stated co-senior author Thomas Wingo, MD. “This is significant because it may explain, at least in part, the well-established epidemiologic link between depression and increased dementia risk.”
Dr. A. Wingo continued, “This relationship begs the question of whether depression treatment can reduce the risk of dementia. We discovered genes that may explain the link between depression and dementia and need additional investigation. Such genes could be important therapy targets for both depression and dementia risk reduction.”
“The expenses of unsuccessful depression treatment continue to rise. There is growing evidence that major depressive disorder raises the chance of Alzheimer’s disease, but there is little understanding of this association” According to John Krystal, MD, Editor of Biological Psychiatry. “This unique work, which connects genetic risk processes to molecular alterations in the brain, provides the clearest evidence to date supporting the concept that depression plays a causative role in Alzheimer’s disease biology.”
This is not to say that if you have a depressive episode, dementia is an unavoidable outcome. Instead, it implies that untreated depression may aggravate the biology of Alzheimer’s disease, potentially hastening the onset of symptoms and increasing the rate of functional loss.”
Scientists do not yet fully comprehend what causes Alzheimer’s disease in the majority of people. The causes are most likely a combination of age-related brain changes, as well as genetic, environmental, and lifestyle factors. The significance of each of these factors in increasing or decreasing the risk of Alzheimer’s disease varies from person to person.
Alzheimer’s disease is a brain disorder that worsens with time. It is characterized by abnormalities in the brain, such as amyloid plaques and neurofibrillary, or tau, tangles, which cause neuronal and neurofibrillary connections to be lost. These and other changes have an impact on a person’s ability to remember and think, as well as their ability to live independently.
Scientists are discovering how age-related changes in the brain might destroy neurons and alter other types of brain cells, so contributing to Alzheimer’s disease damage. These age-related changes include brain atrophy (shrinking), inflammation, vascular damage, the development of unstable chemicals known as free radicals, and the breakdown of energy production inside cells. Age is, however, only one risk factor for Alzheimer’s disease. Many people live into their 90s and beyond and never get dementia.