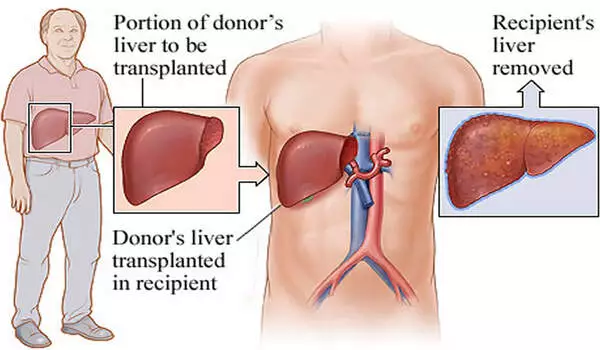
Living donor transplantation is a safe option for liver transplant patients. A healthy person donates a portion of their liver to a recipient in need in this procedure. One of the major benefits of living donor transplantation is that it shortens the waiting period for a liver transplant. Unlike deceased donor transplants, which often require patients to wait for an extended period of time, living donor transplants can be scheduled at a time that is convenient for both the donor and the recipient.
The demand for donor livers for transplant patients exceeds supply, with more than 15% of waitlist patients dying after a year. A new international study supports increasing the use of living donor liver transplantation (LDLT) in Western countries and reducing the organ supply-demand imbalance. Elsevier publishes the Journal of Hepatology, the official journal of the European Association for the Study of the Liver.
LDLT is a procedure in which a portion of a healthy living person’s liver is removed and transplanted into someone whose liver is no longer functioning properly. Within a few months of the surgery, the donor’s remaining liver regrows and returns to normal size, volume, and capacity. Despite the fact that the waiting period for a deceased donor transplant can last up to five years, LDLT is still uncommon in Western countries when compared to those in Asia.
This study provides support for increasing the use of LDLT in Western countries because it provides an opportunity to reduce the imbalance between organ supply and demand and, as a result, offers waitlist candidates the possibility of earlier transplantation and decreased mortality on the transplant waitlist.
Dr. Gonzalo Sapisochin
Identifying differences in outcomes and other transplant characteristics may aid in identifying areas for healthcare improvement and clarifying whether expanding LDLT practices can be justified in countries where DDLT is the primary treatment option.
“There has been a growing interest in strategies to alleviate the increasing demand for transplantation and the unacceptably high mortality on the liver transplant waitlist,” Gonzalo Sapisochin, MD, Ph.D., MSc, Division of General Surgery, University Health Network, Toronto, ON, Canada, explained. “LDLT is one such approach, which can increase the number of grafts available for transplantation. However, both short- and long-term outcomes for donors and recipients must be maintained. We wanted to compare donor and recipient characteristics as well as post-transplant outcomes after LDLT.”
This is a retrospective multicenter study of adults aged 18 and up who had primary LDLT between January 2008 and December 2018, as reported by three national liver transplantation registries: the United Network for Organ Sharing (UNOS; US), the National Health Service Blood and Transplantation (NHSBT; UK), and the Canadian Organ Replacement Registry (CORR; Canada). Patients who were undergoing retransplantation or multi-organ transplantation were not eligible. The researchers compared the three registries’ recipient and donor characteristics, temporal trends, and post-LDLT outcomes. They also wanted to compare the outcomes of LDLT and DDLT in each of the countries.
A total of 2,954 LDLTs were performed in these countries, 2,328 of which took place in the US, 529 in Canada, and 97 in the UK. Canada performed the highest proportion of LDLT procedures over time. Investigators were pleasantly surprised to see that long-term outcomes were excellent despite relatively low use of LDLT in Western countries. The one-, five-, and 10-year patient survival rates were 92.6%, 82.8%, and 70.0% in the USA; 96.1%, 89.9%, and 82.2% in Canada; and 91.4%, 85.4%, and 66.7% in the UK, respectively.
This LDLT analysis shows that, despite the fact that LDLT is used less frequently in Western countries than in Asian countries, long-term survival is excellent. Furthermore, there is no statistically significant difference in mortality risk between these three countries.
“This study provides support for increasing the use of LDLT in Western countries because it provides an opportunity to reduce the imbalance between organ supply and demand and, as a result, offers waitlist candidates the possibility of earlier transplantation and decreased mortality on the transplant waitlist,” Dr. Sapisochin explained.