Research developed antibodies against many rapidly evolving strains of HIV
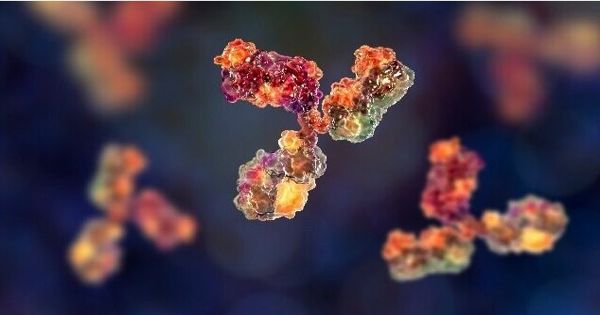
Engineered immune cells produce a large response to HIV in mice, providing hope for a vaccine. Unlike so many other lethal viruses, the vaccine still lacks HIV. The virus—which continues to infect millions around the world—has proved particularly difficult to avoid with traditional antibodies, partially because it is growing very rapidly in the body. Any cure will involve coaxing the body to develop a specific form of antibody that can act broadly to defeat several strains of the virus at once.
Global transmission of the human immunodeficiency virus (HIV) and human suffering left AIDS a global focus. Scientists at Scripps Research have stepped closer to achieving the Holy Grail of HIV research with a novel vaccination strategy that will focus on genetically modified immune cells from the patient’s body. But the ability of HIV to mutate and develop quickly has made the battle against this virus an enormous challenge. Although the challenges to developing a successful HIV vaccine are daunting, progress has been made on several fronts with the development of innovative vectors, adjuvants, and antigen design strategies.
Scientists in Scripps research have developed an approach that has succeeded in producing antibodies against many rapidly evolving strains of HIV. Scientists have moved closer to attaining that goal with an approach that would rely on genetically engineered immune cells from the patient’s body.
In studies involving mice, the method successfully induced broadly neutralizing antibodies—also known as bnabs—that can prevent HIV infection, says Senior Investigator James Voss, PhD, Scripps Science. The research is published in Nature Communications. In 2019, Voss and his team demonstrated that it was possible to reprogram the antibody genes of the B-cell immune system using CRISPR so that the cells would develop the same broadly neutralizing HIV antibodies that were observed in uncommon HIV patients.
The new study reveals that such engineered B cells, after being reintroduced to the body, will replicate in response to vaccination-and mature into memory cells and plasma cells that develop high levels of defensive antibodies over a long period of time in the body. The team also showed that engineered genes can be enhanced to produce antibodies that are much more efficient against the virus, using a mechanism that usually exists in B cells that respond to immunization.
“This is the first time it has been shown that modified B cells can create a durable engineered antibody response in a relevant animal model,” Voss notes. He hopes that his vaccine strategy can someday avoid new HIV infections and potentially provide a functional treatment for those who already have HIV/AIDS. The virus is still present globally, with an estimated 38 million people living with the disease in 2019.
Voss states that in humans, the starting cells for the vaccine could conveniently be collected from a single blood sample, which was then designed in the lab before being reintroduced to the patient. He and his team—including first author Deli Huang, Ph.D., Jenny Tran, PhD, Alex Olson, Ph.D., and graduate student Mary Tenuta—are now researching ways to develop technology to make it available to the largest number of people. Since the method depends on supplying genes to the patient’s own immune cells, this may be a big obstacle.
“People think of cell therapies as being very expensive,” Voss says. “We’re doing a lot of work towards trying to make the technology affordable as a preventative HIV vaccine or functional cure that would replace daily antiviral therapy.”