Ribosomes are protein-synthesizing cellular structures that are involved in the production of proteins required for the maintenance, growth, and repair of the heart muscle. Ribosomes, on the other hand, do not switch the heart between maintenance and energy-boost modes.
Researchers discovered that cardiomyocytes and skeletal muscle cells replace their existing ribosome stock with a different type that can make physical contact with mitochondria, and the cells’ batteries, and significantly increase ATP production. The natural mechanism in the heart is activated in response to myocardial infarction and cardiac hypertrophy. The findings establish ribosomes as a new frontier for therapeutic strategies aimed at preventing or healing heart damage.
The Centre for Genomic Regulation (CRG) in Barcelona has discovered a mechanism involving ribosomes that allows the heart to switch between a ‘regular maintenance mode’ for day-to-day function and an ‘energy-boost mode’ that aids recovery from high-demand situations such as heart attacks. The findings are published in a ‘Breakthrough Article’ in the journal Nucleic Acids Research.
Ribosomes are the molecular factories in all living cells that produce proteins. Historically, they were thought to be simple but necessary workhorses that lacked the ability to regulate cell function. However, there is mounting evidence that these fundamental units, which come in a variety of shapes and sizes, perform specialized tasks that have yet to be discovered.
For a long time, we thought that ribosomes were the same in every single cell of the human body. This makes them impractical drug targets as you could be healing one body part while damaging many others.
Dr. Eva Novoa
The researchers discovered that cardiomyocytes, the cells responsible for heart contraction, and skeletal muscle cells, which are connected to bones and are critical for strength and movement, have different types of ribosomes than all other types of cells in the body using various experimental techniques and cutting-edge sequencing technologies.
“For a long time, we thought that ribosomes were the same in every single cell of the human body. This makes them impractical drug targets as you could be healing one body part while damaging many others. The existence of specialized ribosomes and their specificity to heart and muscle cells is a turning point because it means it is possible to develop medicines that target specific ribosomes for the purpose of treating cardiovascular disease,” explains Dr. Eva Novoa, corresponding author of the study and researcher at the Centre for Genomic Regulation.
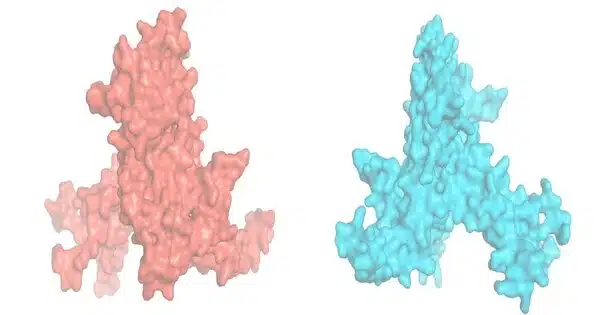
Ribosomes are protein-based structures. While most human cells’ ribosomes contain ribosomal protein L3 (RPL3), cardiomyocytes and skeletal muscle cells’ ribosomes contain ribosomal protein L3-like (RPL3L). The tail is the key distinction between the proteins, which share 77% of their amino acid sequence. According to the findings, cells will only use one of the proteins. Whatever protein is used, the corresponding tail sticks out on the ribosome’s surface, changing its shape and surface, which affects how it binds to other proteins and receptors.
The researchers found that cardiomyocyte and skeletal muscle ribosomes showed no benefit in terms of protein synthesis compared to other ribosomes. However, the researchers were surprised to find that knocking the RPL3L gene out in mice showed both cardiomyocytes and skeletal muscle cells creating ribosomes with RPL3 instead. In stark contrast, knocking out RPL3 was lethal.
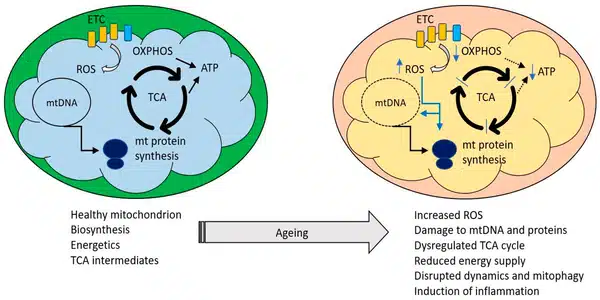
Researchers discovered that this newly discovered compensation mechanism occurred naturally in response to a heart attack or myocardial infarction, with cardiomyocytes replacing all of their existing stock of RPL3L-containing ribosomes with RPL3-containing ribosomes instead. The new ribosomes’ unique shape allows them to physically interact with mitochondria, the cells’ batteries, significantly increasing the production of ATP, the universal currency used for energy. The effect was detected six hours after the infarction and peaked 72 hours later.
This ribosome replacement mechanism also occurs during cardiac hypertrophy, which is a physiological response of the heart to increased workload that can be either physiological, such as after exercise, or pathological, caused by disease. In response to cardiac hypertrophy, RPL3-containing ribosomes in cardiomyocytes peak after 96 hours.
The research sheds light on why the heart and muscle use RPL3L for ribosomes in the first place. The researchers discovered that RPL3L is only found in the ribosomes of adult cardiomyocytes, whereas RPL3 is only found in fetal tissues. Simultaneously, mice lacking RPL3L had lower lean muscle mass at 55 weeks of age than mice with RPL3L.
“When we are born, our hearts require a lot of energy to develop. Cardiomyocytes only express RPL3 at this point, switching to RPL3L once the heart is fully mature. We don’t know why, but the cells may be switching to fine-tune mitochondrial activity in resting conditions and possibly reduce levels of free radicals, which are dangerous byproducts of mitochondrial metabolism. “This could explain how the heart delicately balances two different modes — one in which ribosomes boost energy levels and one in which the heart is kept in maintenance mode,” explains the study’s first author, PhD candidate Ivan Milenkovic.
This mechanism’s discovery can be used to improve cardiac health and function, and it establishes ribosomes as a new frontier for therapeutic strategies that prevent or heal heart damage. The researchers are now delving deeper into the molecular mechanisms that distinguish pathological from physiological cardiac hypertrophy, including mouse exercise tests to see how the presence or absence of RPL3L in cardiomyocytes affects physical performance.