Mendelian randomization, a tool in genetic study, was used to evaluate 12 coagulation parameters, revealing four that are linked with migraine risk. Migraine patients appear to be at higher risk of stroke, and a new study may help explain why.
One idea holds that persons who suffer from migraines acquire hardened plaque within their arteries, known as atherosclerosis, earlier than those who do not suffer from migraines. Atherosclerosis is a primary cause of stroke. This, however, was not observed in the study, which was the first to use high-resolution ultrasound to test the idea.
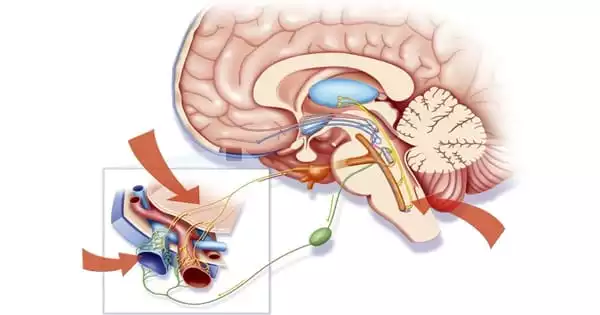
Migraine affects over 15% of the population in the United States. Migraine with aura is a poorly recognized variant of migraine (MA). Individuals suffering from MA frequently notice flashing lights, blind spots, or jagged lines in their visual field prior to the beginning of migraine headaches. Individuals who have MA are also at a higher risk of stroke and cardiovascular illness, though experts are still investigating why this is the case.
In a new study from Brigham and Women’s Hospital, researchers utilized a genetic analysis technique known as Mendelian randomization to investigate 12 coagulation parameters, discovering four that are linked to migraine risk. Interestingly, scientists only noticed these connections in those who have MA and not in people who have migraine without aura (MO). Their findings show that these hemostatic variables may play a causative role in MA. They reported their findings in the journal Neurology.
We’ve always wondered why persons with MA have a higher risk of stroke and other cardiovascular problems. This investigation provides potential MA-specific leads. Finding a plausible etiology of migraine with aura has long been an unanswered subject in the field.
Daniel Chasman
“We’ve always wondered why persons with MA have a higher risk of stroke and other cardiovascular problems,” said corresponding author Daniel Chasman, Ph.D., of the Brigham and Women’s Hospital’s Division of Preventive Medicine. “This investigation provides potential MA-specific leads. Finding a plausible etiology of migraine with aura has long been an unanswered subject in the field.”
For some time, researchers have speculated about the association between coagulation and migraine risk, although past research has been mainly equivocal. Most people initially get migraines when they are young, such as in childhood or early adulthood. Because past study designs primarily included middle-aged and older persons, researchers have questioned whether coagulation causes migraine or whether there is any causality between these two aspects at all. Using Mendelian randomization, which can support or disprove putative causal effects on a health outcome, scientists discovered evidence for the first time that hemostatic variables may add to the risk of MA.
“Even if we observe a link between migraine and these coagulation variables when we assess both in a population at the same time, we still wonder: Which occurred first?” Pamela Rist, ScD, of the Brigham’s Division of Preventive Medicine, was one of the study’s co-authors. “One of the intriguing aspects of Mendelian randomization is that it allows you to investigate potential causality.”
Researchers used summary statistics from decades of previously collected data from migraine sufferers and non-migraine sufferers. Because the diagnostic criteria for MA and MO differ, they could study these two disorders separately.
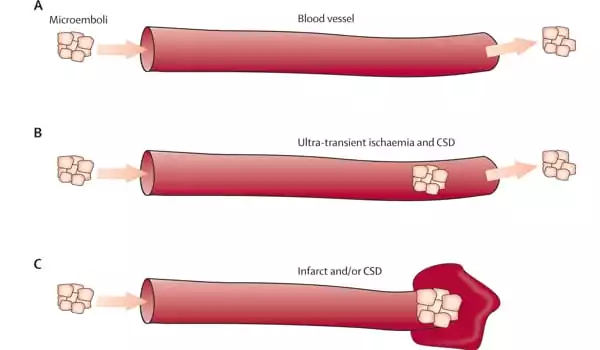
The researchers discovered a robust link between four coagulation variables and migraine vulnerability. They discovered that genetically increased levels of three blood clotting factors, coagulation factor VIII, von Willebrand factor, and phosphorylated fibrinopeptide A, as well as genetically decreased levels of fibrinogen (a protein important in the late stages of the blood clotting process), were all linked to migraine susceptibility. Interestingly, scientists found no correlation between these hemostatic factors and migraine without aura (MO), indicating a particular relationship between these hemostatic factors and MA.
Mendelian randomization has limitations, according to scientists. In the future, researchers could look into whether the causal correlations suggested by genetics can be detected in clinical practice.
“It’s quite interesting that we were able to show that hemostatic variables are connected with MA using Mendelian randomization,” said first author Yanjun Guo, MD, Ph.D. of the Brigham’s Division of Preventative Medicine. “And, because we discovered in the observational studies that MA patients have a higher risk of stroke, these findings could point to a possible link between MA and stroke.”