Pregnancy and childbirth are normal physiological processes that frequently necessitate assistance rather than medical intervention. Pregnancy adaptations include dramatic physiologic changes in all body systems. Many of these changes produce signs and symptoms that can make distinguishing normal “discomforts of pregnancy” (or postpartum) from changes that would be concerning in a nonpregnant adult more difficult.
Access to timely care during maternal and neonatal emergencies remains a complex problem for millions of people living in rural communities in Sub-Saharan Africa. Mfangano Island’s isolated Suba and Luo communities on Lake Victoria in Western Kenya have some of the highest maternal and neonatal mortality rates in East Africa. Researchers from the University of Minnesota have collaborated with one of the world’s most remote and underserved populations to better understand the factors at the heart of this complex challenge.
The Monitoring Maternal Emergency Navigation and Triage on Mfangano (MOMENTUM) Study, published in Global Public Health, employs an innovative adaptive design to assess the delays and barriers faced by mothers and newborns seeking emergency care.
For millions of people living in rural communities in sub-Saharan Africa, accessing timely care during maternal and neonatal emergencies remains a complex problem.
Since 2018, Charles Salmen, MD, director of the Mfangano Community Health Field Station and assistant professor in the Department of Family Medicine and Community Health at the Medical School, and Co-Principal Investigator Louisa Ndunyu, Ph.D., of Maseno University in Kenya, have mentored a team of local and international investigators to launch the MOMENTUM Study.
Simultaneously, the study was intended to provide pragmatic, actionable data to support a locally directed health navigation program serving this remote population. A group of local and international researchers conducted a 12-month mixed-methods cohort study to assess barriers and delays among patients seeking care for pregnancy-related, obstetric, and neonatal emergencies at nine remote health centers on Mfangano Island Division.
“The start of the COVID-19 pandemic in the middle of our data collection period nearly derailed the study. Despite this, we persevered to ensure that the harrowing stories of these mothers and their families were preserved and understood, thanks to the ingenuity and dedication of our team on the ground and remote support from our team at the University of Minnesota “Salmen stated. “Because they were willing to share their experiences from start to finish, this study now represents an important contribution to addressing the vexing problem of maternal emergencies in Sub-Saharan Africa.”
Mfangano Island’s isolated Suba and Luo communities on Lake Victoria in Western Kenya have some of the highest maternal and neonatal mortality rates in East Africa. Researchers from the University of Minnesota have collaborated with one of the world’s most remote and underserved populations to better understand the factors at the heart of this complex challenge.
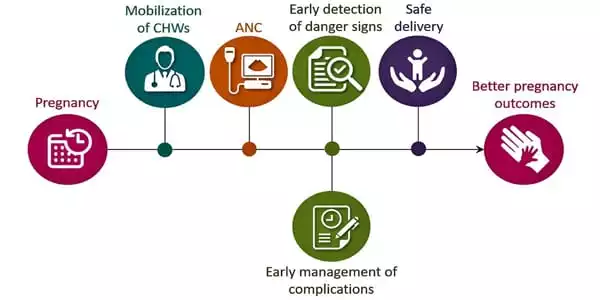
According to the MOMENTUM study, there is an urgent need for community education efforts to raise awareness of emergency conditions, the implementation of streamlined hand-off systems for emergency referrals, and policy-level interventions to address the recurring health worker strikes. The study suggests that community-based care coordinators play an important role, especially in light of frequent facility closures and staffing interruptions.
According to the study, these recurring gaps can be bridged by local interventions that flexibly connect the dots for families and providers across dynamic care environments, synchronizing communication and facilitating timely transport to available resources, and, most importantly, advocating for patients.
With the first round of quantitative data analysis completed, the team in Kenya is now conducting focus group discussions and key informant interviews to better understand how the COVID-19 pandemic has impacted maternal and neonatal emergency care on Lake Victoria. This study is led by Kenyan researchers from Maseno University, local research staff at the Ekialo Kiona Center, and a team of University of Minnesota medical and public health students providing remote support.
The goal of maternal care levels is to reduce maternal morbidity and mortality, including existing disparities, by encouraging the growth and maturation of systems for the provision of risk-appropriate maternal health care. This classification system establishes levels of maternal care that pertain to basic care (level I), specialty care (level II), subspecialty care (level III), and regional perinatal health care centers in order to standardize a complete and integrated system of perinatal regionalization and risk-appropriate maternal care (level IV).
Regional and state health care entities, national accreditation, and professional organization guidelines identified regional perinatal health care service needs, and regional resources should all be considered when determining the appropriate level of care to be provided by a given facility.















