Researchers from the University of Toronto and the University Health Network have demonstrated how probiotic bacteria in the stomach might impair immunity in pancreatic cancer patients, pointing to more customized cancer treatments.
Lactobacillus, a type of bacterium thought to support gut health, can affect the activity of immune cells known as macrophages in the pancreatic tumor environment and encourage cancer growth, according to the findings.
“Most research focus on positive associations between the microbiome and cancer outcomes,” said Tracy McGaha, an immunology professor at the University of Toronto’s Temerty Faculty of Medicine and a senior scientist at the Princess Margaret Cancer Centre, University Health Network. “This study focuses on unfavorable associations of the microbiome with cancer and implies that the microbiome constituency may have a deleterious impact in specific circumstances.”
Macrophages are tissue-resident immune cells that have been linked to tumor growth and metastasis. Lactobacillus influences macrophage function by metabolizing dietary tryptophan, an important amino acid found in protein from both plant and animal sources, according to the study.
Most research focus on positive associations between the microbiome and cancer outcomes. This study focuses on unfavorable associations of the microbiome with cancer and implies that the microbiome constituency may have a deleterious impact in specific circumstances.
Tracy McGaha
Indoles, a type of metabolite produced by microbial tryptophan metabolism, activate the aryl hydrocarbon receptor, or AHR, a protein that regulates gene expression and can cause both helpful inflammation and immunological suppression in other parts of the body.
The researchers discovered that deleting or inhibiting AHR in macrophages resulted in decreased pancreatic cancer growth, improved susceptibility to therapies, and higher numbers of inflammatory T cells. These positive benefits were blocked when AHR was activated.
McGaha expressed astonishment that the microbiome had such a profound influence on AHR and immunological function. “At first, we didn’t think about the microbiome; we were only interested in AHR as a factor in the tumor microenvironment,” McGaha explained. “However, blocking the mammalian genes that activate AHR had little effect.”
The researchers turned to Lactobacillus since prior research had showed that the bacteria connected with AHR activity and lowered inflammation, both of which can promote cancer growth. Working in the University of Toronto’s germ-free animal facility and in partnership with Dana Philpott, an immunology professor, they evaluated the bacteria’s effects in mice with surgical models of pancreatic cancer.
They further advanced the research with single cell analysis, a tool that offers genome-scale data on individual cells and was a significant appeal for McGaha when he moved to Toronto from the United States in 2015.
“The technology was novel at the time, but it’s been invaluable for us to see population responses in macrophage and other immune cell gene expression patterns, as well as what’s going on around them.”
Later, the researchers used tissue samples and data from human trials to demonstrate that high AHR expression corresponds with disease progression, immune suppression, and patient survival.
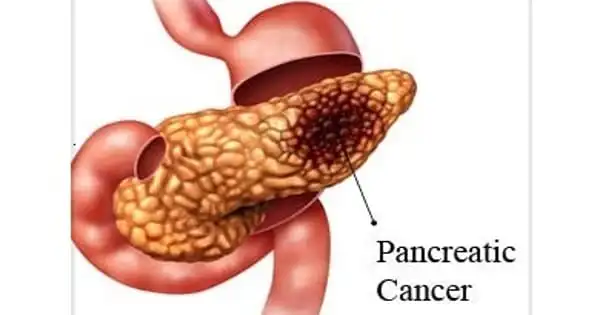
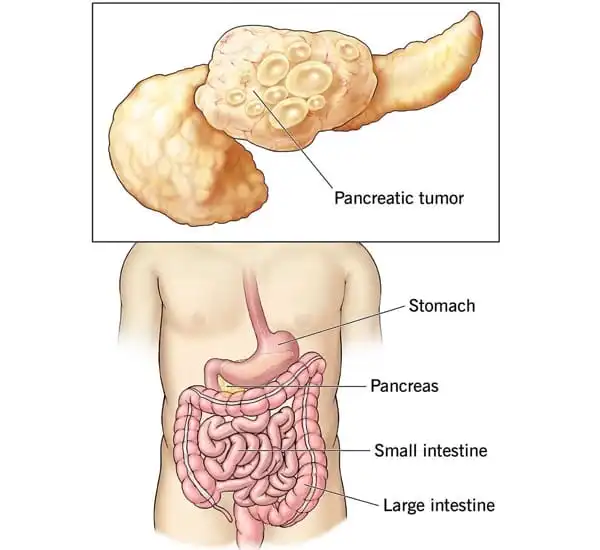
The treatment of pancreatic cancer is notoriously challenging. Despite being relatively rare, it is the third-most lethal cancer in Canada, and patients with the disease have not achieved the survival gains seen in other malignancies over the last three decades.
McGaha is collaborating with clinician scientists at UHN on a clinical trial called PASS-01 to assist address the pressing need for new effective treatments. The study, which is being conducted in partnership with other cancer centers in Canada and the United States, attempts to identify individualized indicators of patient response to treatment. The researchers will collect stool samples before and after chemotherapy to examine for Lactobacillus enrichment, as well as if the bacterium correlates with treatment response, patient survival, and their findings on how it operates in the tumor environment.
“It’s interesting as a fundamental scientist to be part in translational research, and it’s good to see physician scientists interested in this work,” McGaha said. Longer term, McGaha’s lab will work to gain a better knowledge of how immune cells interact with the microbiome. The objective is to improve on promising medicines such as fecal microbiota transplants, which have been limited by the complexity and variety of gut bacteria, or to try a new strategy.
“It may be able to avoid the need to modify the microbiome by precisely directing the immune response to microbial metabolites,” said McGaha. “That’s an exciting new direction we’d want to pursue.”