Scripps Research scientists conducted promising early testing of a new technique that could one day be used to prevent or treat type 2 diabetes. The researchers examined an experimental drug named IXA4 on obese mice, and their findings were published in Nature Communications. They demonstrated that the chemical stimulates a natural signaling system that protects the mice from detrimental, obesity-induced metabolic alterations that would ordinarily result in diabetes.
“With this one molecule, we were able to activate this pathway in both the liver and the pancreas, which added up to a large overall improvement in metabolic health of obese animals,” explains Scripps Research’s Luke Wiseman, PhD. “This is the first time that anyone has demonstrated that a small chemical stimulating this route in this manner works to treat sickness in a live animal,” says Enrique Saez, PhD.
There is currently no cure, however our researchers are working on a groundbreaking weight management trial to assist people put their type 2 diabetes into remission. Remission occurs when blood glucose (or blood sugar) levels return to normal. This does not mean that diabetes is no longer a problem. It is nevertheless critical for persons in remission to get frequent medical checkups. However, being in remission can change your life.
The work was a partnership between the laboratories of Saez and Wiseman, both professors in Scripps Research’s Department of Molecular Medicine and co-senior authors on the new publication.
IRE1/XBP1s signaling is a reaction to cellular stress, and having it on all the time effectively tells the cell that the stress cannot be resolved, so the cell kills itself.
Luke Wiseman
Type 2 diabetes is still a serious public health issue, with an estimated 30 million individuals suffering from it in the United States alone. It is primarily caused by overweight and obesity, and it results in a lack of normal blood sugar management, as well as a slew of health issues such as increased risks of heart disease, stroke, kidney disease, nerve damage, retinal degeneration, and several malignancies. There are numerous medicines available to treat type 2 diabetes, but none of them work well for every patient.
Wiseman’s team has been examining a signaling pathway including two proteins termed IRE1 and XBP1s for several years. When activated by a certain sort of cellular stress, IRE1 activates XBP1s, which affects the activity of a slew of genes, including many metabolic genes, in an attempt to alleviate the cellular stress. Previous research suggests that, at least in the short term, the activity of this pathway can protect liver and fat cells from the pressures induced by obesity – stresses that might injure these cells in ways that promote diabetes.
However, the IRE1/XBP1s pathway is not a clear diabetes medication target. Previous study has demonstrated that keeping IRE1/XBP1 turned on indefinitely harms cells, causes inflammation, and worsens overall metabolic failure.
“IRE1/XBP1s signaling is a reaction to cellular stress, and having it on all the time effectively tells the cell that the stress cannot be resolved, so the cell kills itself,” Wiseman explains.
The immune system destroys insulin-producing beta cells in the pancreas in type 1 diabetes. This implies you can’t produce the insulin you require to survive. To reverse type 1 diabetes, we must cease the immune system’s attack on beta cells. And our scientists are hard at work on it. They hope to create and test immunotherapies, which target the immune system to prevent it from eliminating beta cells.
The current study found that IXA4, a chemical discovered a few years ago, stimulates IRE1/XBP1s for only a few hours at a time. Because it otherwise permits IRE1 to turn off, it can theoretically be administered daily without causing the detrimental signaling seen with persistent IRE1 activation, making it an intriguing option for human therapy.
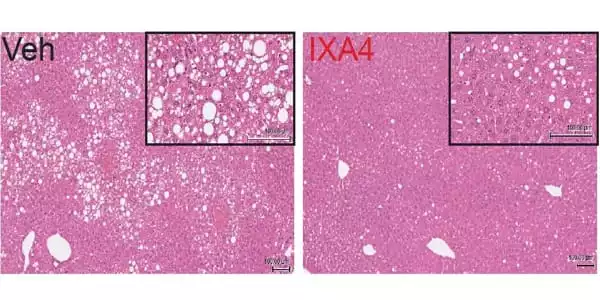
The researchers utilized IXA4 to treat obese mice fed a high-fat, high-calorie diet. When compared to untreated obese mice, the treated mice had improved glucose metabolism and insulin activity, less fat buildup and inflammation in the liver, and no loss of insulin-producing cells in the pancreas after only eight weeks.
Because IXA4 can only reach a limited number of tissues, including the liver and pancreas, the team is currently working on alternative chemicals that can reach a broader range of cells, including fat cells. “We’re also working with IXA4 as a potential treatment for other metabolic illnesses like fatty liver disease,” Saez explains.














