Colorectal cancer, also known as bowel cancer or rectal cancer, is a type of cancer that develops in the colon or rectum (parts of the large intestine). Blood in the stool, changes in bowel movements, weight loss, and fatigue are all possible signs and symptoms. It is the second leading cause of cancer death in men and women in the United States. It is the third most common cause of cancer death in men and the third most common cause of cancer death in women. Colorectal cancer can often be cured if detected early.
According to a new study, artificial intelligence can detect and diagnose colorectal cancer from tissue scans as well as or better than pathologists. According to a new study published in the journal Nature Communications, a Tulane University researcher discovered that artificial intelligence can detect and diagnose colorectal cancer from tissue scans as well as or better than pathologists.
The study, conducted by researchers from Tulane, China’s Central South University, the University of Oklahoma Health Sciences Center, Temple University, and Florida State University, was designed to see if AI could be used to help pathologists keep up with the growing demand for their services.
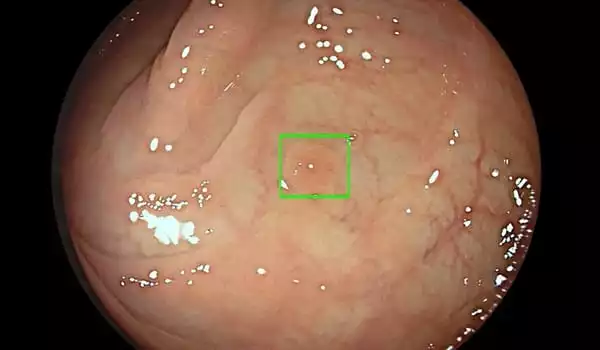
During a colonoscopy, the AI-enabled system places green squares around potential lesions and alerts clinicians with a low-volume sound that additional examination may be required. This study is groundbreaking because we successfully used artificial intelligence to identify and diagnose colorectal cancer in a cost-effective manner, which could ultimately reduce pathologists’ workload.
Dr. Hong-Wen Deng
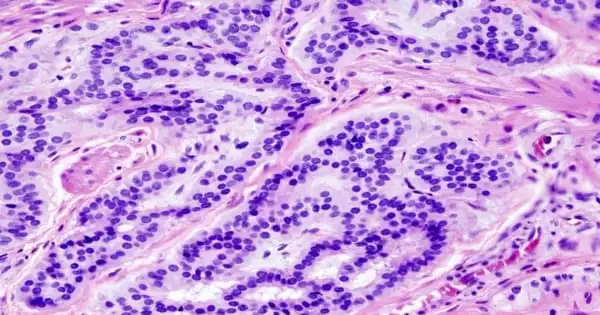
Pathologists regularly evaluate and label thousands of histopathology images to determine whether someone has cancer. However, their average workload has increased significantly, which can sometimes lead to unintentional misdiagnosis due to fatigue.
During a colonoscopy, the AI-enabled system places green squares around potential lesions and alerts clinicians with a low-volume sound that additional examination may be required. According to the FDA, the system is not intended to diagnose or instruct clinicians on how to manage suspicious polyps.
“Even though much of their work is repetitive, most pathologists are extremely busy because there is a huge demand for what they do, but there is a global shortage of qualified pathologists, particularly in many developing countries,” said Dr. Hong-Wen Deng, professor and director of Tulane University School of Medicine’s Tulane Center of Biomedical Informatics and Genomics. “This study is groundbreaking because we successfully used artificial intelligence to identify and diagnose colorectal cancer in a cost-effective manner, which could ultimately reduce pathologists’ workload.”
Deng and his colleagues collected over 13,000 colorectal cancer images from 8,803 subjects and 13 independent cancer centers in China, Germany, and the United States for the study. Using images chosen at random by technicians, they created a machine-assisted pathological recognition program that allows a computer to recognize images of colorectal cancer, which is one of the leading causes of cancer-related deaths in Europe and America.
“The difficulties in this study stemmed from the complex large image sizes, complex shapes, textures, and histological changes in nuclear staining,” Deng explained. “However, the study concluded that when we used AI to diagnose colorectal cancer, the performance was comparable to, if not better than, that of real pathologists in many cases.”
Deng and his team used the area under the receiver operating characteristic (ROC) curve, or AUC, as a performance measurement tool to determine the study’s success. The study discovered that the average pathologist scored.969 for accurately identifying colorectal cancer manually after comparing the computer’s results with the work of highly experienced pathologists who interpreted data manually. The average score for the machine-assisted AI computer program was.98, which is comparable to, if not more accurate than, human intelligence.
Using artificial intelligence to detect cancer is a new technology that has not yet gained widespread acceptance. Deng hopes that the study will lead to more pathologists using prescreening technology to make faster diagnoses in the future.
The majority of colorectal cancers are adenocarcinomas. These cancers begin in cells that produce mucus to lubricate the colon and rectum. When doctors discuss colorectal cancer, they almost always refer to this type. Some subtypes of adenocarcinoma, such as signet ring and mucinous, may have a poorer prognosis (outlook) than others.
“We are still in the research phase, and we have not yet commercialized it because we need to make it more user friendly and test and implement it in more clinical settings. However, as we develop it further, we hope to be able to use it for different types of cancer in the future. Using AI to diagnose cancer can speed up the process and save time for both patients and clinicians.”