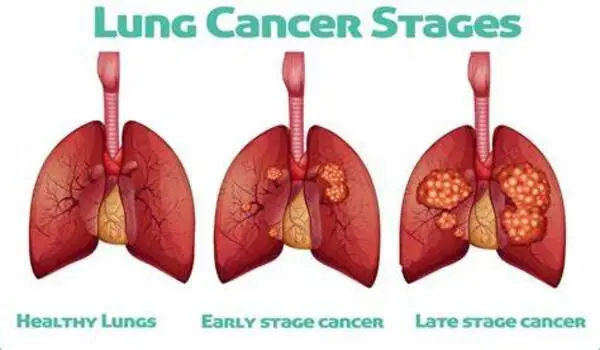
Lung cancers known as adenocarcinomas can sometimes respond to initially effective treatments by converting into a much more aggressive small cell lung cancer (SCLC), which spreads quickly and has few treatment choices. Weill Cornell Medicine researchers created a mouse model to shed light on this problematic process known as histological transition. The findings add to our understanding of how altered genes might drive cancer evolution and propose targets for more effective treatments.
The researchers, whose findings were published in Science on February 8, discovered that during the transition from lung adenocarcinoma to small cell lung cancer (SCLC), the mutated cells appeared to change cell identity via an intermediate, stem cell-like state, facilitating the transformation.
“It is very difficult to study this process in human patients. So my aim was to uncover the mechanism underlying the transformation of lung adenocarcinoma to small cell lung cancer in a mouse model,” said study lead Dr. Eric Gardner, a postdoctoral fellow in the laboratory of Dr. Harold Varmus, the Lewis Thomas University Professor of Medicine and a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. The complex mouse model took several years to develop and characterize but has allowed the researchers to crack this difficult problem.
It is very difficult to study this process in human patients. So my aim was to uncover the mechanism underlying the transformation of lung adenocarcinoma to small cell lung cancer in a mouse model.
Dr. Eric Gardner
This study was in collaboration with Dr. Ashley Laughney, assistant professor of physiology and biophysics and a member of the Meyer Cancer Center at Weill Cornell Medicine, and Ethan Earlie, a graduate student in the Laughney lab and part of the Tri-Institutional Computational Biology and Medicine program.
“It is well known that cancer cells continue to evolve, especially to escape the pressure of effective treatments,” said Dr. Varmus. “This study shows how new technologies — including the detection of molecular features of single cancer cells, combined with computer-based analysis of the data — can portray dramatic, complex events in the evolution of lethal cancers, exposing new targets for therapeutic attack.”
Catching Transformation in the Act
SCLC most commonly occurs in heavy smokers, but this type of tumor also develops in a significant number of patients with lung adenocarcinomas, particularly after treatment with therapies that target a protein called Epidermal Growth Factor Receptor (EGFR), which promotes tumor growth. The new SCLC-type tumors are resistant to anti-EGFR therapy because their growth is fueled by a new cancer driver, high levels of Myc protein.
To better understand the interplay of different cancer pathways, the researchers altered mice to produce a common kind of lung adenocarcinoma in which lung epithelial cells are driven by a mutant version of the EGFR gene. They next transformed the adenocarcinoma tumors into SCLC-type tumors, which often develop from neuroendocrine cells. They accomplished this by inhibiting EGFR in the presence of numerous additional alterations, including the deletion of the tumor suppressor genes Rb1 and Trp53, as well as increasing the production of Myc, a recognized driver of SCLC.
Oncogenes, like EGFR and Myc, are altered versions of genes that typically regulate cell growth. They are well-known for contributing to cancer’s growth and spread. Tumor suppressor genes, on the other hand, normally inhibit cell proliferation and tumor development.
Context Matters
Surprisingly, this study showed that oncogenes act in a context-dependent manner. While most lung cells are resistant to becoming cancerous by Myc, neuroendocrine cells, are very sensitive to the oncogenic effects of Myc. Conversely, epithelial cells, which line the air sacs of the lungs and are the precursors to lung adenocarcinomas, grow excessively in response to mutated EGFR.
“This shows that an ‘oncogene’ in the wrong cell type doesn’t act like an oncogene anymore,” Dr. Laughney said. “So, it fundamentally changes how we think about oncogenes.”
The researchers also uncovered a stem cell-like intermediate that wasn’t an adenocarcinoma or SCLC. Cells in this transitional state became neuroendocrine only after the tumor suppressor genes RB1 and TP53 were mutated. They discovered that the loss of another tumor suppressor called Pten accelerated the process. At that point, oncogenic Myc may induce these intermediate stem-like cells to develop SCLC-type malignancies.
This work lends credence to efforts to develop therapies that target Myc proteins, which have been linked to a variety of malignancies. The researchers intend to use this new mouse model to further investigate the adenocarcinoma-SCLC transition, including how the immune system often responds to this change.