Human stem cells and a bioengineered scaffold were used by researchers at the Francis Crick Institute and University College London (UCL) to reconstruct a human thymus. The thymus is a crucial immune system organ, and the accomplishment is a significant step toward creating an artificial thymus for transplant treatment. “Showing it is possible to build a working thymus from human cells is a crucial step towards being able to grow thymi which could one day be used as transplants,” said Sara Campinoti, a researcher at the Crick Institute’s Epithelial Stem Cell Biology and Regenerative Medicine Laboratory.
Reporting in Nature Communications (“Reconstruction of a functional human thymus by postnatal stromal progenitor cells and natural whole-organ scaffolds,”)”This is an important proof-of-principle that a long-lived phenocopy of a human thymus using only postnatal, cultivated cells is achievable.”
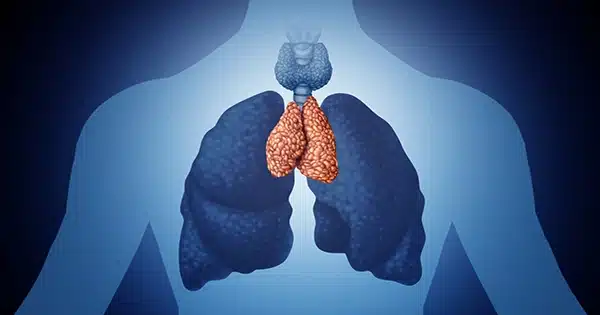
The thymus, a main lymphoid organ that is situated in the chest, is “critical for T cell maturation and selection,” according to the scientists. Severe immunodeficiency, in which the body is unable to combat infectious diseases or cancerous cells, or autoimmunity, in which the immune system mistakenly attacks the patient’s own healthy tissue, can result from thymus dysfunction or failure to develop during fetal development. The researchers added, “Since the thymus regulates the development of immune competence and tolerance, its functional dissection and subsequent reconstruction with desired cell populations might provide powerful tools applicable to a variety of medical conditions, including primary or acquired immune deficiencies.”Indeed, such is the clinical unmet need that cultivated thymus slices are currently used for transplantation into athymic patients.”
However, attempts to construct a completely functional thymus have had “limited success,” according to the scientists, probably due to the organ’s complexity. However, there has been considerable “uncertainty” regarding whether this might be accomplished utilizing postnatal epithelial stem/progenitor and mesenchymal cells, and if so, if such cells could be grown in sufficient quantities ex vivo. The scientists detail how they effectively regenerated thymi using stem cells collected from patients who had to have the organ removed during surgery in their newly published proof-of-concept research. When bioengineered thymi were transplanted into mice, they were able to foster the formation of mature and functioning human T cells. While researchers have previously rebuilt other organs or sections of organs, the team suggests this is the first time that scientists have successfully rebuilt a whole working human thymus.
The thymi from patients who underwent open chest heart surgery were collected by the researchers, and in the lab, thymic epithelial cells (TEC) and thymic interstitial cells (TIC) from the donated tissue were grown into multiple colonies of billions of cells to produce the whole organ. The next stage was to acquire a structural thymic scaffold, which they could then fill with the cultivated thymic cells. In order to do this, co-author Asllan Gjinovci, a senior laboratory research scientist at the Crick, created a novel method to clear rat thymi of all cells, leaving just the structural scaffolds. For this, the researchers had to employ a novel microvascular surgical strategy because the thymus cannot be successfully treated using standard techniques.
Gjinovci commented, “This new approach is important because it enables us to obtain scaffolds from larger organs like the human thymus, something essential to bringing this beautiful work to the clinic.”
The researchers then injected up to six million thymic epithelial cells and thymic interstitial cells from the lab colonies into the organ scaffolds. The cells grew onto the scaffolds, and after just five days, the organs resembled those observed in a nine-week-old fetus. “… organ-size, 3D structures that supported the survival and appropriate spatial organization of thymic stromal cells, facilitating thymocyte differentiation,” the scientists said.
The scientists discovered that the lab-grown thymi could encourage the formation of human lymphocytes in over 75% of transplants when they placed them into “humanized” mice. Roberta Ragazzini, a postdoctoral research scientist at the Crick Institute and co-author of the study, added, “It’s incredibly fascinating that we can substantially increase thymic stem cells obtained from human donors into enormous colonies. It enables the procedure to be scaled up such that “human size” thymi may be built.
The team believes the study is significant not just for future research into and treatment of severe immune deficiencies, but also for creating novel approaches for growing artificial organs more generally. “The data described in this study demonstrate that postnatal human thymus harbors epithelial (TEC) and interstitial (TIC) cells that can expand to clinically relevant numbers in vitro, suitable for contributing to the reconstruction of a human functional thymus in vivo,” the scientists stated. Our findings provide realistic prospects for treating immunological illnesses such as congenital athymia, for which existing treatments are restricted, by overcoming hurdles to establishing a functioning thymus using just enlarged, postnatal donor stromal cells.”
The procedure for reconstructing thymi is still being improved and scaled up by scientists. Paola Bonfanti, senior author and group head at the Crick and professor in the division of infection and immunity at UCL, said, “Our work has other potential future applications in addition to providing a new source of transplants for people without a working thymus.” “For instance, while the thymus aids in the immune system’s ability to distinguish between self and non-self, it presents a challenge for organ transplants because it may prompt the immune system to fight the transplant. We might be able to get around this by additionally transplanting a thymus that was generated again using cells from the donor’s thymus. We are optimistic that this will keep the body from fighting the transplant. The study is still in its early stages, but it is an interesting idea that might eliminate the need for patients to take immune suppressors for the rest of their lives.”
Source: https://www.genengnews.com/news/scientists-create-whole-functional-thymus-from-human-cells/