WEHI researchers discovered an enzyme in the thymus that is required for immunological T cells to accurately identify threats, preventing them from becoming rogue and destroying healthy tissue in the body.
The thymus is a vital organ in which immunological T cells learn how to combat infection. According to the latest results, the enzyme KAT7 is required to activate thousands of genes required for ‘teaching’ immune T cells not to assault healthy tissue. Immune T cells are at risk of undermining the immune system if they are not properly trained, which could lead to autoimmune diseases such as Type 1 diabetes or multiple sclerosis.
The study, which was published in Science Immunology, paves the path for new medicines that target KAT7, which could adjust the training of immunological T cells as needed. Such treatments could be used to either prevent immune T cells from causing autoimmune illnesses or to boost immune T cells to help them fight diseases like cancer.
Dr. Melanie Heinlein, a former WEHI PhD student, led the study with Associate Professor Tim Thomas and Associate Professor Daniel Gray from WEHI, as well as academics from Monash University and the Weizmann Institute of Science in Israel.
KAT7 acts as a training coordinator, directing AIRE to the thousands of genes that must be active in order for the ‘boot camp’ to go well. KAT7 does this by marking the genes that AIRE requires to ‘turn on’ in order for the majority of the body’s proteins to function.
Dr. Melanie Heinlein
At a glance
- Researchers revealed that the enzyme KAT7 is critical for ‘training’ immunological T cells to recognize and fight dangers in the body.
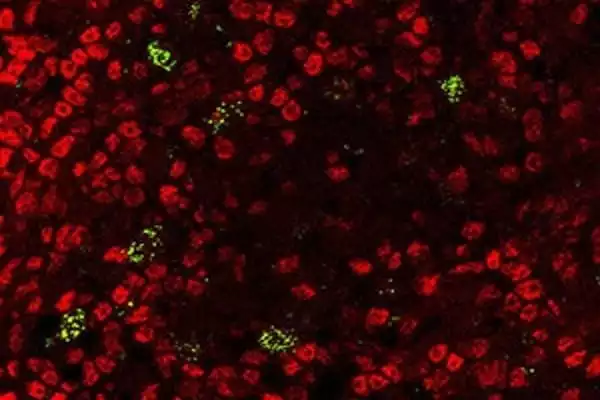
- They demonstrated that inhibiting KAT7 activity in pre-clinical mice caused the immune system to go into overdrive, resulting in a variety of autoimmune diseases.
- These findings suggest that KAT7 could be targeted therapeutically to either depress or stimulate the immune system, depending on the situation.
A ‘preview’ of threats
The thymus functions as a ‘boot camp’ for immunological T cells, teaching them to recognize and fight viruses while also teaching them not to assault healthy organs. Immune T cells are provided a “preview” of all the different components of healthy tissues they may meet once they escape the thymus as part of this preparation. While it was previously known that the Autoimmune Regulator (AIRE) protein activated the hundreds of genes required for this preview, until now it was unclear how AIRE understood which genes to ‘turn on.’
The new discoveries, according to Dr. Melanie Heinlein, demonstrated that the enzyme KAT7 was critical for recognizing which genes AIRE needed to activate in order for immunological T cells to be correctly educated.
“KAT7 acts as a training coordinator, directing AIRE to the thousands of genes that must be active in order for the ‘boot camp’ to go well. KAT7 does this by marking the genes that AIRE requires to ‘turn on’ in order for the majority of the body’s proteins to function. When everything goes as planned, immunological T cells are educated not to attack any normal tissues they may encounter in the body, preventing autoimmune illness” She stated.
Importance of KAT7
KAT7’s critical role in keeping immunological T cells on task, according to Associate Professor Tim Thomas, was highlighted when the researchers used a new medication to disrupt its function.
“We demonstrated how a KAT7 inhibitor developed in partnership with Jonathan Baell at Monash University was able to prevent AIRE from turning on the genes required for appropriate immunological T cell training. Stopping this process threw the immune system into overdrive, resulting in renegade immunity T cells and a variety of autoimmune diseases in pre-clinical mice. This demonstrates a clear relationship between KAT7 and AIRE in immunological tolerance maintenance “He stated.
“This has been a fantastic team effort. The highly collaborative work was made possible by expertise from WEHI’s Flow Cytometry Laboratory, Genomics Facility, and Centre for Dynamic Imaging, as well as colleagues from Monash University and Israel’s Weizmann Institute of Science.”
Exciting treatment potential
According to Associate Professor Daniel Gray, the discovery could lead to new medicines for suppressing immune T cells to avoid autoimmune diseases or supercharging immune T cells to fight disease.
“According to our findings, KAT7 could be targeted to adjust the training of immunological T cells, allowing them to be either halted from producing autoimmunity or encouraged to fight disease. This understanding could be used to treat organ-specific autoimmune illnesses like Type 1 diabetes and multiple sclerosis, as well as cancer immunotherapy. By suppressing KAT7 in the thymus, the immune system could be supercharged to attack cancer in the latter situation “He stated.
Professor Jacques Miller AC FRS FAA contributed to the funding of this research. In 1958, Professor Miller identified the function of the thymus, which changed our knowledge of the immune system, infection, and disease. It is his discovery that has allowed for future thymus research, like as this current study.