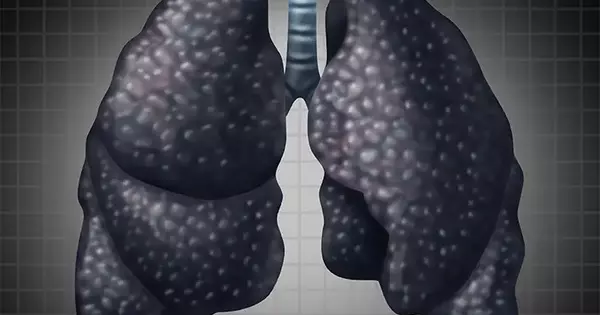
According to a new study that compared the pathology and mineralogy of the disease across generations, silica exposure is a driving force behind rising rates of coal workers’ pneumoconiosis. The study provides scientific evidence for why progressive massive fibrosis, the most severe form of black lung disease, is becoming more common and prevalent among younger coal workers in West Virginia, Virginia, and Kentucky.
According to a new study published by occupational health experts at the University of Illinois Chicago and their collaborators, silica exposure is a driving force behind rising rates of coal workers’ pneumoconiosis.
The research is the first to compare the pathology and mineralogy of the disease, also known as black lung disease, across generations. It is also the first to provide scientific evidence for why progressive massive fibrosis, the most severe form of black lung disease, is becoming more common and prevalent among younger coal workers in West Virginia, Virginia, and Kentucky.
Prior to 2005, when the increase was first reported, the incidence of black lung disease had been declining since the 1970s, when modern coal dust controls were implemented. Following investigations, it was discovered that black lung cases had tripled and that tenured miners in central Appalachia, the disease’s epicenter, had experienced a tenfold increase in severe black lung disease.
Our findings highlight the importance of controlling workplace silica exposure to prevent the disabling and untreatable adverse health effects afflicting US coal miners.
Dr. Robert Cohen
“We knew silica is highly toxic and that it contributes to coal workers’ pneumoconiosis, but we didn’t know why coal workers were suddenly experiencing more disease and more severe forms of it. Because regulations have not changed, minerals in the Earth have not changed, and there is no evidence that people have become more vulnerable to coal dust, the rise in cases among young workers that began in the late 1990s was perplexing” Dr. Robert Cohen, clinical professor of environmental and occupational health sciences at UIC and director of the Mining Education and Research Center, echoed this sentiment.
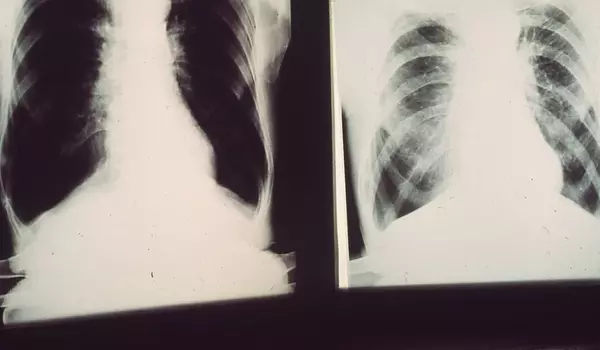
Cohen and his colleagues collected lung tissue samples from coal miners suffering from severe black lung disease in order to better understand this phenomenon. They compared samples from miners born between 1910 and 1930 to those born in or after 1930, resulting in historical and “contemporary” coal miners.
The pathology of the samples — the physical characteristics of the diseased lungs — was examined by the researchers. Tissues with more than 75% silicotic nodules, which are round with whirls of pinkish scar tissue, were classified as having silica-type disease; tissues with less silicotic nodules and a greater number of grey or black-pigmented nodules were classified as having coal-type (less than 25%) or mixed-type disease (25 percent -75 percent). They also looked for other lesions, such as mineral dust-related alveolar proteinosis, which is caused by silica exposure and manifests as fluid-like material on lung tissue.
The chemistry, crystal structure, and physical properties of the mineral particles in the samples were measured using advanced analytical techniques such as scanning electron microscopy and X-ray spectroscopy.
Cohen and his team found a clear link between silica exposure and severe black lung disease in contemporary miners:
- When compared to their historical counterparts, modern miners had significantly higher rates of silica-type disease (57 percent vs. 18 percent ). Historical miners, on the other hand, had a significantly higher proportion of coal-type (50 percent vs. 17 percent) and mixed-type (33 percent vs. 26 percent) diseases.
- Mineral dust alveolar proteinosis was more prevalent in modern miners (70 percent vs. 37 percent).
- The percentage (26 vs. 18%) and concentration (4.7 vs. 2.6 billion particles per cubic centimeter) of silica particles in modern miners were significantly higher.
- The concentration of silica particles was significantly greater (more than 50%) when silica-type severe black lung, mineral dust alveolar proteinosis, silicotic nodules or immature silicotic nodules were present.
“These findings provide the first direct evidence that silica is a causative agent behind the increasing incidence of progressive massive fibrosis – severe black lung disease. This is critical information that can be used to determine health-protective permissible exposure limits for coal miners,” Cohen said.
He attributes silica-driven resurgence to mining technology changes, such as mechanized coal extraction devices introduced in the United States in the 1950s, when miners born in or after 1930 would have begun their careers. “Silica is a mineral found in rock, and technology that allows for more profitable mining below and above the coal seam means more cutting through rock and more silica exposure,” he explained.
“Our findings highlight the importance of controlling workplace silica exposure to prevent the disabling and untreatable adverse health effects afflicting US coal miners,” Cohen and his colleagues write.
The Mine Safety and Health Administration initiated a request for information in 2019 to inform its silica rules, but the 1969 standard remains in effect. The rule allows for 100 micrograms of silica exposure per cubic centimeter. The Occupational Safety and Health Administration, which sets occupational health standards for nearly all other industries, allows 50 micrograms per cubic centimeter.
The findings were published in the Annals of the American Thoracic Society article, “Pathology and Mineralogy Demonstrate Respirable Crystalline Silica is a Major Cause of Severe Pneumoconiosis in US Coal Miners.”