Brain cancer, particularly malignant gliomas, has been a difficult disease to treat due to the complexity of the brain and the difficulty of targeting cancer cells while preserving healthy brain tissue. If scientists discover a hidden weakness specific to deadly brain cancer, it could lead to significant advances in treatment and improved patient outcomes.
The difficult-to-treat brain cancer glioblastoma steals a person’s mental faculties as it spreads, but the tumor’s insidious ability to infiltrate neighboring networks in the brain could also prove fatal.
UC San Francisco researchers discovered that neural activity in these lethal tumors can restructure connections in surrounding brain tissue, causing the cognitive decline associated with the disease, and that the drug gabapentin, commonly used to prevent seizures, could block this growth-causing activity in glioblastoma mice. The findings, published in Nature, point to a promising new direction for research into a disease that has defied even the most advanced and sophisticated cancer drugs.
“Glioblastoma needs a win,” said neurosurgeon Shawn Hervey-Jumper, MD, who co-led the research with postdoctoral scholar Saritha Krishna, Ph.D. “This study opens up a whole new world of treatment options for these patients, as well as a new way of thinking about brain cancer.”
Gabapentin actually kept the tumor from expanding. This gives us hope that combining gabapentin with other glioblastoma therapies will help to prevent some of the cognitive decline we see in patients and possibly extend their lives.
Saritha Krishna
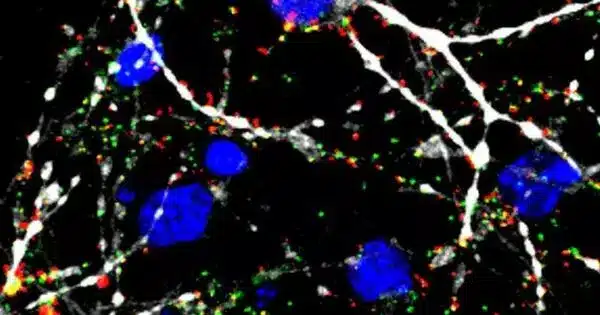
When Hervey-Jumper started his research, scientists had just discovered that brain tumors are fed by a positive feedback loop. Cancer cells begin to produce substances that can act as neurotransmitters. This “extra” supply of neurotransmitters causes neurons to become hyperactive, which promotes cancer cell growth.
Hervey-Jumper focused on what the feedback loop meant for human behavior and cognition in brain cancer, building on previous research on mice and brain organoids (small bundles of neurons derived from human stem cells grown in petri dishes).
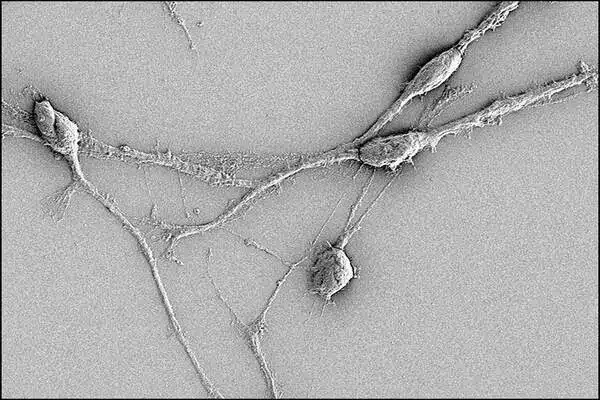
The volunteers were awaiting surgery for glioblastoma tumors that had infiltrated the brain region controlling speech. Hervey-Jumper placed a grid of tiny electrodes on the surface of the speech region just before operating on the tumor, then showed the volunteers pictures and asked them to name what they saw.
The researchers then compared the findings to normal-appearing non-tumor brain regions from the same participants. They discovered that the tumor-infiltrated brain regions of the participants used a broader neural network of brain areas to identify what they were seeing.
Cancer as a Conversation Between Cells
According to Hervey-Jumper, this is due to a decrease in information-processing power in that region of the brain. He compares it to an orchestra, where the musicians playing in unison make the music work.
“If you lose the cellos and woodwinds, the remaining players just can’t carry the piece the way they could otherwise,” he explained. The brain cells trapped in the tumor are so damaged that others from further away must be recruited to perform tasks that were previously controlled by a smaller area.
The study shows that it is the interaction of cells that causes the cognitive decline associated with brain cancer, not inflammation and tumor growth, as scientists previously thought.
“A brain tumor isn’t just sitting there dying,” said Hervey-Jumper. “It’s being regulated by the nervous system. It’s having conversations with the cells around it and actively integrating into brain circuits, remodeling the way they behave.”
We Haven’t Thought About Cancer in This Way
The researchers now knew that the tumors were exploiting the brain’s networks. So they tested gabapentin in mice engrafted with human glioblastoma cells, which controls seizures by tamping down excess electrical activity in the brain.
“Gabapentin actually kept the tumor from expanding,” Krishna explained. “This gives us hope that combining gabapentin with other glioblastoma therapies will help to prevent some of the cognitive decline we see in patients and possibly extend their lives.”
The findings are likely to be applicable to other types of neural cancer, such as those of the spine, and may help explain why the brain is the first site of metastasis in many cancers. According to Hervey-Jumper, the study encourages cancer specialists to consider cell communication networks, such as the positive-feedback loop in glioblastoma, as potential treatment targets, in addition to genetic and immunological approaches.
“We haven’t thought about cancer in this way before,” he explained. “The idea that cancer cells and healthy brain cells can communicate is something of a paradigm shift.”