Alzheimer’s disease is thought to be caused by an abnormal protein buildup in and around brain cells. Amyloid is one of the proteins involved, and deposits of it create plaques around brain cells. Tau is the other protein, and deposits of it form tangles within brain cells. Although the actual cause of this process is unknown, scientists now know that it begins several years before symptoms manifest.
According to scientists, heart disease can directly induce brain malfunction early on, which can lead to dementia, and it can triple the quantity of an Alzheimer’s protein in the brain. The new study, published in the journal eLife, discovered that heart illness causes a breakdown of a fundamental brain function that connects brain activity and blood flow, resulting in the brain receiving less blood for the same level of activity.
This occurs in heart disease patients prior to the accumulation of fat in the blood arteries of the brain (atherosclerosis) and is a precursor to dementia. It was previously unknown how some forms of vascular dementia may occur years before atherosclerosis in the brain.
The researchers also observed that combining heart problems with a genetic susceptibility to Alzheimer’s Disease triples the quantity of beta-amyloid, a protein that builds up and promotes Alzheimer’s, and raises the amounts of an inflammatory gene (IL1) in the brain.
Alzheimer’s disease is the most common form of dementia worldwide, and heart disease is a key risk factor for both Alzheimer’s and dementia. The new discoveries will help us better understand the relationship between heart disease and dementia.
Dr. Osman Shabir
Tens of billions of neurons—specialized cells that process and send information via electrical and chemical signals—are found in a healthy human brain. They communicate between different areas of the brain as well as between the brain and the muscles and organs of the body. Alzheimer’s disease affects this connection between neurons, resulting in functional loss and cell death.
In healthy aging, the brain shrinks to some extent but, surprisingly, does not lose a substantial number of neurons. However, with Alzheimer’s disease, the damage is widespread, with many neurons ceasing to function, losing connections with other neurons, and dying. Alzheimer’s disease impairs processes that are essential to neurons and their networks, such as communication, metabolism, and repair.
Alzheimer’s disease often damages neurons and their connections in memory-related areas of the brain, such as the entorhinal cortex and hippocampus, at first. Later, it affects parts of the cerebral cortex that are responsible for language, logic, and social interaction. Many other parts of the brain are eventually affected. A person with Alzheimer’s disease gradually loses his or her ability to live and function independently over time. In the end, the sickness is fatal.
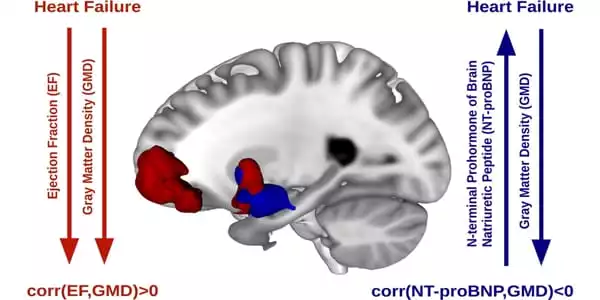
“Alzheimer’s Disease is the most common form of dementia worldwide, and heart disease is a key risk factor for both Alzheimer’s and dementia,” said Dr. Osman Shabir of the University of Sheffield’s Neuroscience and Healthy Lifespan Institutes. The new discoveries will help us better understand the relationship between heart disease and dementia. We observed that midlife heart disease triggers the breakdown of neurovascular coupling, a critical system in our brains that regulates the quantity of blood delivered to our neurons. This breakdown implies that the brain does not get enough oxygen when it is needed, which can lead to dementia over time.”
Neurons are important players in the central nervous system, but other cell types are equally important for optimal brain function. In fact, glial cells outnumber neurons in the brain by a factor of ten. These cells, which exist in a variety of types, including as microglia, astrocytes, and oligodendrocytes, surround and support the function and health of neurons. Microglia, for example, protect neurons from physical and chemical harm and are in charge of removing foreign substances and cellular detritus from the brain. Glial cells frequently work with blood arteries in the brain to carry out these duties. Glial and blood vessel cells work together to maintain the delicate balance within the brain, ensuring that it operates optimally.
The British Heart Foundation has recently offered the team a three-year funding to investigate the use of an arthritis treatment that targets IL1 to determine if it can reverse or minimize the brain dysfunction seen to be caused by heart disease. The researchers also discovered that brain traumas can impair cerebral blood flow regulation, lending credence to previous observations that patients’ symptoms frequently increase following injuries or falls.