Schwann cells, which are widespread in the peripheral nervous system and form a protective sheath around nerve fibers, have been revealed to have an important role in migraine pain by an international team of researchers. Their research shows how pain is conveyed from within Schwann cells and identifies multiple strategies to inhibit this transmission, potentially revealing targets for new migraine treatments.
Migraines impact more than 15% of adults, with women being twice as likely as men to suffer from these severe headaches. Calcitonin gene-related peptide (CGRP), a tiny protein in the neurological system, is recognized to have an essential role in migraine pain; in fact, a new generation of migraine medications uses monoclonal antibodies to target CGRP or its receptor.
“While CGRP has been linked to migraine pain, the mechanism by which it induces pain has been a source of debate in the scientific community,” said Nigel Bunnett, Ph.D., professor and chair of the Department of Molecular Pathobiology at NYU College of Dentistry. Bunnett co-led the study with Pierangelo Geppetti, MD, professor of clinical pharmacology at the University of Florence and director of the Careggi University Hospital’s Headache Center.
Calcitonin gene-related peptide (CGRP), a tiny protein in the neurological system, is recognized to have an essential role in migraine pain. The efficacy of CGRP monoclonal antibodies for migraine and the inability of antibodies to pass the blood-brain barrier suggests that CGRP produces pain in the periphery rather than within the brain.
Professor Nigel Bunnett
“The efficacy of CGRP monoclonal antibodies for migraine and the inability of antibodies to pass the blood-brain barrier suggests that CGRP produces pain in the periphery rather than within the brain,” Bunnett, an NYU Pain Research Center researcher, stated.
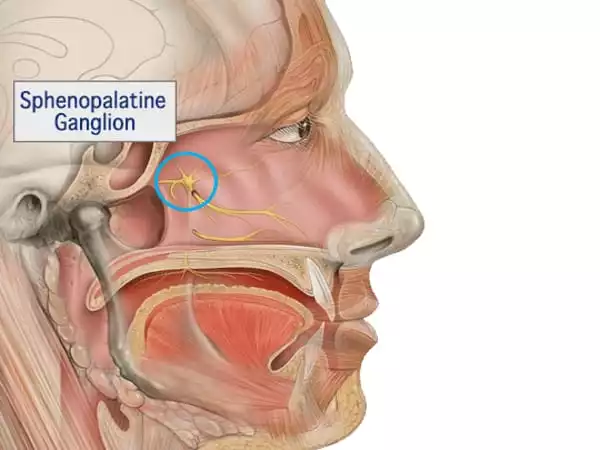
Bunnett and his colleagues focused on Schwann cells, which are present outside the brain in the peripheral nervous system, to investigate the biological mechanism of CGRP-evoked pain. The researchers looked at mice that had the CGRP receptor, known as CLR/RAMP1, impaired in Schwann cells. They altered the CGRP receptor by removing RAMP1, one of the receptor’s two key components, from Schwann cells in the mouse’s face.
CGRP administration rendered the facial region of normal mice extremely sensitive, acting as a surrogate for migraine pain. CGRP, on the other hand, did not cause pain in animals lacking the CGRP receptor in Schwann cells. In a subsequent experiment, the researchers used capsaicin, a substance found in hot chili peppers. Capsaicin stimulates an ion channel called TRPV1, which triggers the release of CGRP and, as a result, pain. Again, capsaicin did not elicit migraine-like pain in mice lacking the CGRP receptor in Schwann cells, lending credence to the notion that the CGRP receptor in Schwann cells plays an important role in migraine pain.
The researchers then uncovered what happens within human Schwann cells to signal pain. When CGRP attaches to its receptor on a Schwann cell, the receptor travels into a compartment within the cell known as an endosome. The CGRP receptor continues to signal for extended periods of time within endosomes. This signaling produces nitric oxide, a pain mediator, which is then released from the Schwann cell and interacts with an ion channel called TRPA1 on a neighboring neuron. TRPA1 stimulates the neuron and sends pain signals.
This new understanding of how pain begins within Schwann cells provided the researchers with two treatment options for migraine pain: preventing the CGRP receptor from accessing endosomes in the first place, or employing nanoparticles to deliver medications targeting the CGRP receptor in endosomes.
The researchers blocked clathrin and dynamin, two proteins involved in the transport of chemicals into cells, to keep CGRP receptors out of endosomes. Inhibiting clathrin and dynamin decreased pain signaling, suggesting a possible target for new migraine therapies.
The researchers also used nanoparticles to encapsulate a small molecule medication that binds to and blocks the CGRP receptor, which successfully suppressed CGRP-evoked pain. While most medications only reach the cell’s surface, nanoparticles can be created to assist medicine in reaching the endosome within a cell and releasing the drug once it arrives. The nanoparticles delivered the medication into the endosomes of Schwann cells, where it blocked the CGRP receptor, thereby inhibiting migraine pain.
“While the significance of CGRP in migraine pain is widely established, this is the first study to specifically link Schwann cells to migraine pain. Based on our improved understanding of how pain is signaled from within endosomes, it offers prospective new techniques to treating migraine” Bunnett stated.
The researchers are collaborating with many partners, including the National Institutes of Health’s National Center for Advancing Translational Sciences, to continue exploring the use and safety of nanoparticle drug delivery before these treatments may be evaluated in humans.
















