According to a new study in mice conducted by researchers at Washington University School of Medicine in St. Louis, an investigational cancer medication that deprives tumors of their energy supply also shows promise of enhancing whole-body metabolism, leading to improved weight control. The findings were published in Cell Reports Medicine.
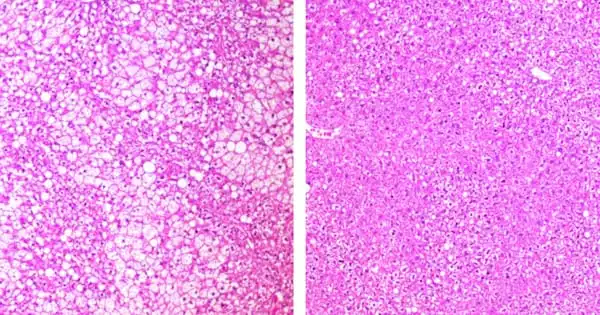
Treatment with the medication ADI-PEG 20 raised insulin sensitivity, improved cholesterol levels, reduced fat deposition in the liver, and reduced inflammation in a group of mice genetically predisposed to obesity and a different group of mice that became obese due to a high-fat, high-sugar diet. Treatment with the medicine prevented the mice, who were genetically predisposed to fat from birth, from gaining the typical amount of weight. Treatment with the medicine resulted in weight loss in mice that had become obese due to a high-fat, high-sugar diet.
The medicine is being researched as a potential treatment for a variety of diseases, including sarcoma, breast, and pancreatic cancer. The medicine degrades the amino acid arginine in the blood, depriving cancer cells of a critical source of fuel. The researchers became interested in examining the drug after discovering that the genes responsible for breaking down arginine are greatly increased while the body is starving. They wondered if the medicine could have the same impact as fasting.
Giving this medicine appears to replicate some of the metabolic and therapeutic consequences of fasting. The magnitude of the effect astounded me. In the mice prone to weight gain, the group that received the medicine weighed around 25% less than the mice who did not get the drug.
Brian DeBosch
Indeed, the researchers discovered that the medication causes cells to go through a process known as autophagy, or self-eating, which is a cellular-level housecleaning activity. Autophagic cells use their own cellular waste products as fuel. During fasting, when no new fuel is coming from the outside, cells shift to autophagy, turning inward for their fuel supply.
“Giving this medicine appears to replicate some of the metabolic and therapeutic consequences of fasting,” said senior author and associate professor of pediatrics Brian DeBosch, MD, Ph.D. “The magnitude of the effect astounded me. In the mice prone to weight gain, the group that received the medicine weighed around 25% less than the mice that did not get the drug. We also noticed similar weight loss from the medication in mice fed a high-fat, high-sugar diet. Furthermore, we do not believe that the majority of the drug’s metabolic benefits are due to changes in body weight. In fact, for several outcome indicators, metabolic alterations came before significant weight changes.”
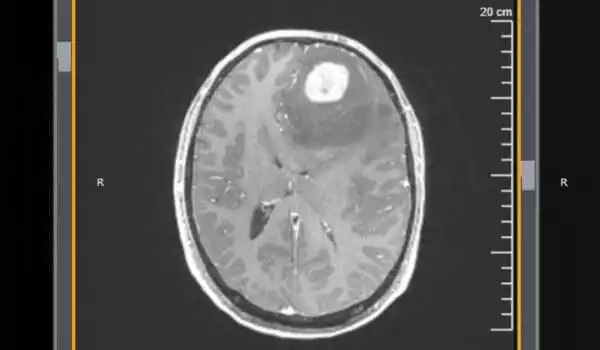
The medicine has been studied in clinical studies for its safety and efficacy in treating a variety of tumor types, including breast, prostate, pancreatic, and liver malignancies. In general, metabolic treatments offer less side effects and are safer than chemotherapy, radiation, and even newer immunotherapies for cancer treatment.
DeBosch, a pediatric gastroenterologist at St. Louis Children’s Hospital, said the research team would like to perform a clinical trial of the medicine to see if it has similar metabolic advantages and weight loss in overweight or obese persons. One unanswered question is whether the medicine is safe to use for an extended period of time. It is not a little chemical that can be used for decades, like a statin. Because the medicine is a protein, it is possible that patients will develop an immunological reaction to it over time. DeBosch, on the other hand, sees a potential role for such a treatment in the coming weeks to months.
“Many obese individuals considering bariatric surgery must first reduce some weight to make the procedure safer,” DeBosch explained. “Such people may find it difficult to shed up to 10% of their body weight before surgery. This form of therapy could potentially act as a bridge to assist patients in losing weight before to bariatric surgery, lowering the risk of complications during and after the procedure.”