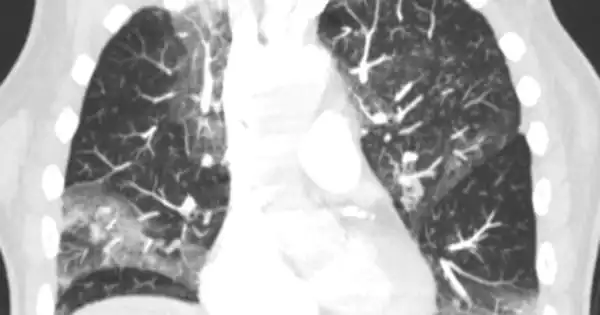
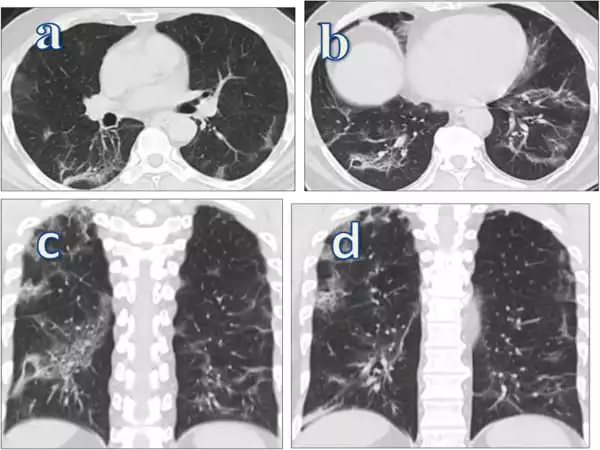
COVID-19 can result in lung complications such as pneumonia and, in severe cases, acute respiratory distress syndrome (ARDS). Another possible complication of COVID-19 is sepsis, which can cause long-term damage to the lungs and other organs. Newer coronavirus variants may also cause increased airway disease, such as bronchitis, which may be severe enough to necessitate hospitalization.
According to a review published in Clinical Microbiology Reviews, a journal of the American Society for Microbiology, a combined treatment strategy targeting SARS-CoV-2 symptoms and severe lung tissue injury is essential to minimize lung sequelae – chronic complications resulting from COVID-19 infection.
COVID-19 can affect the respiratory system in a variety of ways and at varying degrees of severity, depending on a person’s immune system, age, and comorbidities. Symptoms can range from mild to severe, including coughing, shortness of breath, and fevers, as well as respiratory failure, shock, and multi-organ system failure.
According to Huaiyong Chen, Ph.D., principal investigator at Tianjin Institute of Respiratory Diseases and Director of Tianjin Key Laboratory of Lung Regenerative Medicine, Haihe Hospital, Tianjin University, China, therapy using lung epithelial stem and progenitor cells shows promise for mitigating the potentially lethal and highly damaging virus-induced inflammatory storm that can occur in severe cases of COVID-19.
To minimize lung damage, we should promote tissue regeneration efficiently by activating surviving lung stem and progenitor cells, or by directly transplanting healthy lung stem and progenitor cells into damaged lungs.
Huaiyong Chen
“To minimize lung damage, we should promote tissue regeneration efficiently by activating surviving lung stem and progenitor cells, or by directly transplanting healthy lung stem and progenitor cells into damaged lungs,” Chen explained.
Both cell types have the ability to differentiate into lung epithelial cells, which cover the inner surfaces of the lungs where air exchange takes place. They can repair lung damage caused by SARS-CoV-2 in this way, including fibrosis.
Priming the tissue environment with mesenchymal stem cells is the first step in activating these regenerative cells. These cells do not normally reside in the lung, but when transplanted there, they secrete growth factors that help the lung epithelial stem and progenitor cells grow and differentiate. This, in turn, can help to repair the damage. The researchers are currently experimenting with animal models to determine the best way to accomplish this.
In severe cases, however, these regenerative cells may be damaged by cytokines, which are produced in large quantities by immune cells during lung inflammation, preventing complete restoration of lung structure and function.
Healthy stem and progenitor cells may need to be transplanted into a person’s lungs in such cases. However, as with any transplant, immune rejection is a possibility. Chen is investigating the possibility of using CRISPR gene editing technology to modify these cells to reduce immunogenicity prior to transplantation.
It is especially important to note that patients with underlying lung disease can almost certainly have their conditions worsened by contracting or being exposed to COVID-19. COVID-19 can worsen these conditions, such as asthma, chronic obstructive pulmonary disease (COPD), interstitial lung disease, and others.
In less severe cases, researchers will need to look for compounds that increase the ability of progenitor and stem cells to initiate repair and regeneration of the lungs after these injuries. Previous research has shown that certain compounds that target signaling pathways in stem and progenitor cells have the potential to improve lung regeneration in asthma and lung fibrosis patients. They might do the same for SARS-CoV-2 patients.
Pneumonia causes the lungs to fill with fluid and become inflamed, making breathing difficult. Breathing problems in some people can become severe enough to necessitate hospitalization with oxygen or even a ventilator. The pneumonia caused by COVID-19 usually spreads to both lungs. Fluid fills the air sacs in the lungs, limiting their ability to take in oxygen and causing shortness of breath, coughing, and other symptoms.
Chen’s discovery that even 12 years after recovery, some survivors of the closely related virus, Severe Acute Respiratory Syndrome (SARS), first identified in 2003, were living with multiple sequelae, reducing quality of life, prompted the current study. “At that point, I realized that something had to be done to maximize lung regeneration, repair, and recovery,” Chen explained.