Obesity and overweight are on the rise and have become a worldwide epidemic. Obesity has a negative impact on all systems, including reproductive health. Obesity is common in infertile women, and it is well known that there is a link between obesity and infertility. The connection between obesity and reproductive functions is still being researched.
Overweight women are more likely to experience menstrual dysfunction and anovulation. Women who are overweight or obese are at a higher risk of having a miscarriage. In these women, the risk of subfecundity and infertility, conception rates, miscarriage rates, and pregnancy complications is increased.
Obesity is linked to an increased risk of female reproductive disorders; however, the roles and mechanisms of obesity in the cause(s) of reproductive conditions are unknown. A study published in PLOS Medicine by Samvida Venkatesh and colleagues from the University of Oxford in the United Kingdom suggests an etiological link between obesity and a variety of female reproductive conditions, but the extent of this link varies by condition.
Obesity has serious implications for the reproductive system, depending on the amount and distribution of body fat. Obesity clearly contributes to menstrual disorders, infertility, miscarriage, poor pregnancy outcome, impaired fetal well-being, and diabetes mellitus, according to epidemiological evidence.
We present genetic evidence that both generalized and central obesity play an aetiological role in a wide range of female reproductive conditions, though the extent of this link varies significantly between conditions. Our findings suggest that there is a need to investigate the mechanisms underlying the causal associations of overweight and obesity on gynaecological health in order to identify targets for disease prevention and treatment.
Samvida Venkatesh
Female reproductive disorders are common conditions that have a negative impact on many people’s health and well-being. Obesity’s role in the development of female reproductive conditions, on the other hand, has received little attention. Researchers conducted a Mendelian randomization study on 257,193 women of European ancestry aged 40-69 to investigate the causal associations between obesity, metabolic hormones, and female reproductive disorders. They accessed records from the UK Biobank, a large-scale biomedical database containing participants’ medical, environmental, and genetic information.
The researchers then developed a statistical model to estimate the relationship between BMI and waist-to-hip ratio and the risk of a variety of female reproductive conditions such as endometriosis, heavy menstrual bleeding, pre-eclampsia, and infertility.
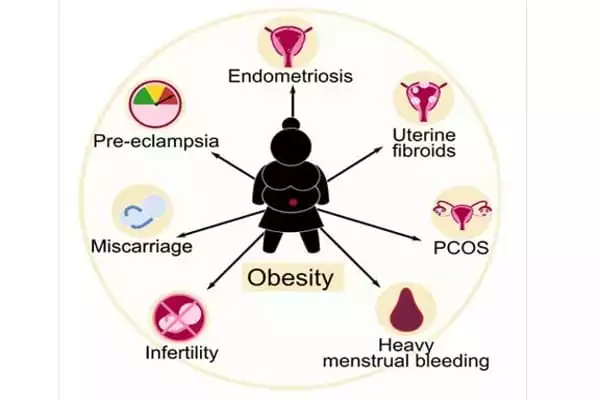
Obesity was linked to a variety of female reproductive disorders, including uterine fibroids, polycystic ovary syndrome, heavy menstrual bleeding, and pre-eclampsia, according to the study’s findings. They also discovered that some inherited genetic variation linked to obesity is also linked to female reproductive disorders, though the strength of those associations varied depending on the type of obesity and reproductive condition. The study had several limitations, including a low prevalence of female reproductive disorders among participants and a lack of prior body mass index and waist-hip-ratio data.
Obesity, a major health concern, is a common issue among women of reproductive age. Obesity and overweight are characterized by abnormal and excessive fat accumulation, which has a negative impact on the body’s health. The World Health Organization (WHO) defines overweight as having a body mass index (BMI) equal to or greater than 25 kg/m2, while obesity is defined as having a BMI equal to or greater than 30 kg/m2.
Obesity causes a slew of issues, including social, psychological, demographic, and health issues. It is associated with increased health risks such as diabetes, hypertension, coronary heart disease, and osteoarthritis, as well as various cancers, most notably endometrium, breast, and colon cancers. Obesity is also linked to reproductive problems, particularly in women. It has been linked to anovulation, menstrual disorders, infertility, difficulty with assisted reproduction, miscarriage, and poor pregnancy outcomes.
The authors claim that “We present genetic evidence that both generalized and central obesity play an aetiological role in a wide range of female reproductive conditions, though the extent of this link varies significantly between conditions. Our findings suggest that there is a need to investigate the mechanisms underlying the causal associations of overweight and obesity on gynaecological health in order to identify targets for disease prevention and treatment.”
Gonadotropin secretion is impaired in obese women due to increased peripheral aromatization of androgens to estrogens. Obese women’s insulin resistance and hyperinsulinemia result in hyperandrogenemia. The levels of sex hormone-binding globulin (SHBG), growth hormone (GH), and insulin-like growth factor binding proteins (IGFBP) fall while leptin rises. As a result, the neuro-regulation of the hypothalamic-pituitary-gonadal (HPG) axis suffers. These changes could explain why ovulatory function is impaired, and thus reproductive health.