While there is no medically recognized treatment for long-term COVID, exercise may help to stop the vicious cycle of inflammation that can lead to diabetes and depression months after the virus has been eradicated.
According to the findings of a new study, adding a 30-minute exercise routine may halt the loop of inflammation that can contribute to the development of at least two post-COVID conditions: diabetes and depression.
“We know that Long COVID causes depression, and we know that it can raise blood glucose levels to the point where people develop diabetic ketoacidosis, a potentially fatal condition common in people with type 1 diabetes,” said Candida Rebello, Ph.D., a research scientist at Pennington Biomedical Research Center. “Exercise can be beneficial. Exercise reduces the inflammation that causes high blood glucose levels, as well as the development and progression of diabetes and clinical depression.”
Long-COVID, also known as post-COVID problems, are being found in an increasing number of individuals more than 4 weeks following infection. According to the Centers for Disease Control and Prevention, patients with post-COVID disorders have “a constellation of other debilitating symptoms.” Breathing difficulties, shortness of breath, exhaustion, lethargy, postexertional malaise, chest discomfort, stomach pain, headache, heart palpitations, and musculoskeletal pain are the most prevalent long-COVID problems.
We all know that physical activity is an important part of living a healthy life. According to this study, exercise can be used to break the chain reaction of inflammation that leads to high blood sugar levels and, ultimately, the development or progression of type 2 diabetes.
John Kirwan
It is unknown how many people are affected by Long COVID. However, estimates range from 15% to 80% of those afflicted. Based on such data, it’s possible that up to 1 million Louisiana residents have Long COVID.
Long COVID creates “a constellation of other debilitating symptoms” such as cognitive fog, muscle pain, and exhaustion that can linger for months after a person recovers from the original infection, according to the Centers for Disease Control.
“For example, a person may not feel really sick from COVID-19, but six months later, long after the cough or fever has gone away,” Dr. Rebello explained. Exercising is one option. Dr. Rebello and her co-authors discuss their concept in the journal Exercise and Sport Sciences Reviews in “Exercise as a Moderator of Persistent Neuroendocrine Symptoms of COVID-19.”
“You don’t have to sprint or even walk a mile at a rapid pace,” Dr. Rebello explained. “Walking slowly is also a form of exercise. Ideally, you should exercise for 30 minutes. However, if you can only do 15 minutes at a time, split it up into two 15-minute sessions. If all you have time for is a 15-minute walk once a day, do it. The most essential thing is to give it a shot. It makes no difference where you start. You can progressively increase your level of activity until you reach the suggested level.”
“We all know that physical activity is an important part of living a healthy life. According to this study, exercise can be used to break the chain reaction of inflammation that leads to high blood sugar levels and, ultimately, the development or progression of type 2 diabetes” Pennington Biomedical Executive Director John Kirwan, Ph.D., who is also a co-author of the paper, commented.
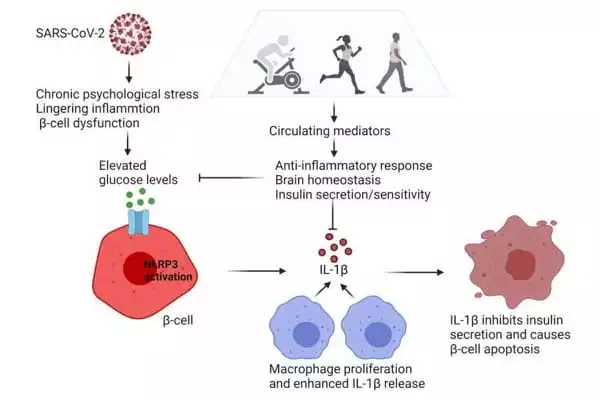
According to the authors, post-acute COVID-19 hyperglycemia is most likely caused by persisting inflammation or chronic psychological stress, which is exacerbated by β-cell dysfunction. Chronic psychological stress disrupts and overactivates the hypothalamic-pituitary-adrenal axis, resulting in sympathetic nervous system activation and an excessive immunological response, which promotes insulin resistance and β-cell dysfunction.
The researchers also discovered that high local concentrations of interleukin-1β (IL-1β) in the β-cell microenvironment limit insulin production, induce -cell malfunction and death, raise glucose levels, and stimulate IL-1β autostimulation.
Patients are not required to “run a mile or even walk a mile at a rapid pace,” according to Dr. Rebello. “Walking slowly is also a form of exercise.” Patients should exercise in 30-minute increments ideally; patients can begin with 15-minute increments and work up to 30-minute sessions, according to Dr Rebello. “What matters is that you try.” It makes no difference where you start. You can progressively increase your level of activity until you reach the suggested level.”
“We all know that physical activity is an important part of living a healthy life. “This study demonstrates that exercise can be used to break the chain reaction of inflammation that leads to high blood sugar levels and, ultimately, the development or progression of type 2 diabetes,” said Pennington Biomedical Executive Director John Kirwan, PhD, who is also a co-author of the paper.