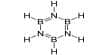
Benzodiazepines are widely medicated, but they are usually recommended for short-term use because long-term use can cause dependence and resistance. Benzodiazepines, sometimes known as “benzos”, are a class of psychiatric drugs whose basic chemical structure is a fusion of a benzene ring and a diazepine ring. The first benzodiazepine, chlordiazepoxide (Librium), was discovered in 1955 and made available for clinical use in 1960 (Sternbach 1972). In 1977 benzodiazepines were the most commonly prescribed drug worldwide. These are in the family of drugs commonly known as drug transciliators. It was approved by the U.S. Food and Drug Administration before 1982 and is still 1 in the top 200 drugs. Although initially intended as worrisome, it now has many more hints.
Benzodiazepines are a group of CNS depressants that experience calm (anxiolysis), sleep, and drowsiness. They work to facilitate inhibitory neurotransmitter GABA binding to various GABA receptors across the CNS. High doses of many short-acting-benzodiazepines can cause anterograde amnesia and isolation. These properties make benzodiazepines useful for treating anxiety, insomnia, movement, convulsions, muscle spasms, alcohol withdrawal, and as a suggestion of treatment or dental procedures. There is no clear distinction between anisiolytics and hypnosis, as most psychotics induce sleep when taken at night and most hypnotics are sedated during the day. Benzodiazepines are classified as short, moderate, or long-acting. Short- and medium-acting-benzodiazepines are preferred for the treatment of insomnia; Long-acting benzodiazepines are recommended for the treatment of anxiety.
Benzodiazepines, also known as minor tranquilizers, are commonly prescribed by doctors to treat and relieve stress and anxiety and help people fall asleep. They can also be used to treat alcohol withdrawal and epilepsy. Adverse reactions can occur, such as the growing movement or panic of minorities. Benzodiazepines are associated with an increased risk of suicide. Long-term use is controversial due to concerns about declining efficacy, physical dependence, withdrawal, and increased risk of dementia and cancer. The combined use of alcohol and benzodiazepines also increases the risk of fatal overdose because of both act as CNS depressants. Similar fatal interactions occur when opium is taken with benzodiazepines as part of the polydruze use pattern. Although they are not the main teratogen, there remains uncertainty as to whether they cause ruptured palate in a small number of infants and whether prenatal exposure causes neurohevicular effects; These are signs of withdrawal in newborns.
Benzodiazepines can cause overdose, especially when used with alcohol or other drugs. Even after a short period of use, they are associated with symptoms of dependence and withdrawal. However, they are less toxic than their predecessors, and barbiturates and benzodiazepines are the only drugs that can rarely cause death. When other central nervous system disorders (CNS) are combined with alcoholic beverages and opioids, the likelihood of toxicity and fatal overdose increases. Benzodiazepine addicts eventually seek the drug of their choice and eventually incur personal costs for themselves and their families, even taking increasingly desperate steps for it.