According to the 2016 Global Burden of Disease Study, migraine is the most common neurological condition, characterized by recurring attacks of headache and numerous sensory complaints, and is rated sixth among the top causes of years lived with disability. Migraine produces a variety of neurological problems, accounting for more than half of the causes of neurological years lived with disability, and contributing to an increasing number of individual- and societal-level burdens as a result of the associated pain and sensitivity.
Migraines are a pain in the head and in the hip pocket, but newly found genetic factors by QUT researchers may pave the way for novel preventative medications and cures. Professor Dale Nyholt and his PhD students Hamzeh Tanha and Anita Sathyanarayanan from the QUT Centre for Genomics and Personalised Health published the results of their genetic analysis in The American Journal of Human Genetics.
According to Professor Nyholt, the researchers discovered genetic correlations to three blood metabolite levels that enhance migraine risk:
- decreased amounts of DHA, an omega-3 fatty acid that has been shown to reduce inflammation
- increased levels of LPE(20:4), a substance that inhibits an anti-inflammatory molecule
- reduced levels of X-11315, a third, as-yet unidentified metabolite.
Observed relationships between genetic factors influencing blood metabolite levels and genetic risk for migraine suggest an alteration of metabolites in people with migraine.
Professor Nyholt
Professor Nyholt believes that future research and clinical trials could target these genetic linkages in order to design and test medicines that change metabolite levels and prevent migraine. According to him, migraine costs the Australian economy $35.7 billion a year, and existing treatments fail up to 50% of migraine patients.
“Observed relationships between genetic factors influencing blood metabolite levels and genetic risk for migraine suggest an alteration of metabolites in people with migraine,” Professor Nyholt said.
Metabolites are compounds produced or utilised by the body during the breakdown of food, medicines, or chemicals during metabolism. “Variations in blood levels of metabolites can be caused by diet, lifestyle, and heredity,” Professor Nyholt explained. “However, they are straightforward to assess and can be controlled by meal planning and supplementation.”
Except for docosahexaenoic acid (DHA), a very long-chain omega-3 that protects against migraine, patients with migraine had higher amounts of shorter length fatty acids, according to Professor Nyholt. “Fatty acids are composed of more complex lipids that aid in cell signaling, cell membrane composition, and gene expression, all of which influence disease risk,” he explained.
“Lower DHA levels are linked to inflammation, cardiovascular and brain problems such as depression, all of which are linked to migraine risk.” According to Professor Nyholt, LPE(20:4) is a chemical substance that inhibits the development of an anti-inflammatory molecule known as anandamide. “If LPE(20:4) is managed to allow more anandamide to be produced to lower inflammation, this could potentially prevent migraine,” he explained.
Lower blood levels of a third metabolite called X-11315, according to Professor Nyholt, also increased the risk of migraine, and characterizing it was a subject of future research.
Migraine is a common primary headache illness that is normally regarded to be harmless. However, anatomical and functional alterations in the brain of migraine patients have been identified. Individuals with migraine show a higher frequency of white matter abnormalities, silent infarct-like lesions, and volumetric changes in both gray and white matter when compared to controls. In both the interictal and ictal phases of migraine, functional magnetic resonance imaging (MRI) investigations revealed disrupted connectivity. MR spectroscopy and positron emission tomography studies reveal that migraine patients have aberrant energy metabolism and mitochondrial malfunction, as well as other metabolic abnormalities.
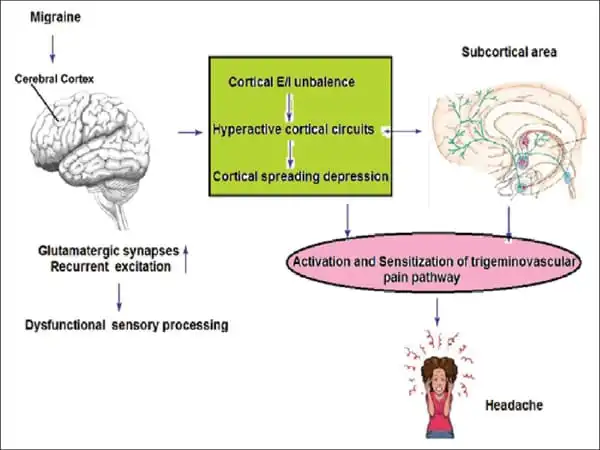
Despite the significant occurrence of migraine, diagnosis is based exclusively on non-specific symptoms and indicators, and there is a lack of a definitive diagnostic tool and approach. While there is still some debate about the pathophysiology of migraine, converging evidence from brain imageology and electrophysiology indicates that migraine is caused by a breakdown in the excitatory-inhibitory balance.














