In a recent innovation, a research team successfully created eye tissue using 3D bioprinting, which is still developing. The tissue that has been produced will be utilized to track the development of age-related macular degeneration and other degenerative retinal eye disorders.
In 3D bioprinting, materials known as bio-inks are deposited layer by layer to produce tissue-like structures that are later employed for medical research.
The 3D bioprinting procedure was developed by the researchers using patient stem cells as the building block. A mixture of cells that make up the outer blood-retina barrier-eye tissue was printed using this method. These are the cells that protect the retina’s photoreceptors, which detect light.
The National Institutes of Health’s National Eye Institute (NEI) in the United States is the source of the invention.
Kapil Bharti, the lead researcher, explains why attention is being paid to this particular tissue: “We know that age-related macular degeneration begins in the outer blood-retina barrier. Due to a paucity of physiologically plausible human models, the processes of age-related macular degeneration beginning and development to advanced dry and wet phases remain poorly understood.
The retinal pigment epithelium forms the outer blood-retina barrier and is separated from it by a region known as Bruch’s membrane (the innermost layer of the choroid of the eye). This separates the membrane from the choriocapillaris, which is rich in blood vessels. An essential job is performed by Bruch’s membrane, which controls the flow of nutrients and waste materials between the choriocapillaris and the retinal pigment epithelium.
When age-related macular degeneration occurs, drusen, or lipoprotein deposits, develop outside of Bruch’s membrane. The membrane’s ability to function is subsequently hampered by these deposits, which ultimately cause vision loss and photoreceptor degradation.
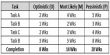
Pericytes and endothelial cells were mixed with two other immature choroidal cell types in a hydrogel for the bioprinting process. All of these are significant capillary components. Fibroblasts were added to this, which gives tissues structure.
The gel was then printed on a biodegradable scaffold by the researchers. The cells developed into a dense capillary network in a few days. The scaffold was seeded with retinal pigment epithelial cells on the ninth day.
On day 42, the printed tissue reached complete maturity and began to function like the natural outer blood-retina barrier. This served as a practical guide for the researchers while they conducted their research on eye conditions.
Making a suitable biodegradable scaffold and producing a reliable printing pattern posed the most technical challenges. These problems were solved by creating a temperature-sensitive hydrogel that, while cold, formed separate rows but disintegrated as it warmed.
The study, titled “Bioprinted 3D outer retina barrier uncovers RPE-dependent choroidal phenotype in advanced macular degeneration,” is published in the journal Nature Methods.