Robot-assisted surgery for bladder cancer excision and reconstruction allows patients to recover much faster and spend significantly (20%) less time in hospital, according to the findings of a first-of-its-kind clinical experiment headed by academics at UCL and the University of Sheffield.
The study, published in JAMA and funded by The Urology Foundation with a grant from the Champniss Foundation, also discovered that robotic surgery cut the risk of readmission in half (52%) and revealed a “striking” four-fold (77%) reduction in the prevalence of blood clots (deep vein thrombus & pulmonary emboli) – a significant cause of health decline and morbidity – when compared to patients who had open surgery.
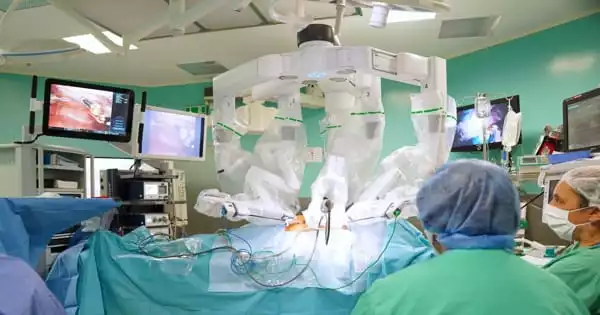
Patients’ stamina and quality of life improved as their physical activity increased, as measured by daily steps tracked on a wearable smart sensor. Unlike open surgery, which includes a surgeon working directly on a patient and significant incisions in the skin and muscle, robot-assisted surgery allows surgeons to remotely guide less invasive instruments using a console and 3D image. It is currently only offered at a few UK hospitals.
The findings, according to the researchers, provide the strongest evidence yet of the patient benefit of robot-assisted surgery, and they are now urging the National Institute of Clinical Excellence (NICE) to make it available as a clinical option across the UK for all major abdominal surgeries, including colorectal, gastro-intestinal, and gynecological procedures.
In this study, we aimed to see if, as compared to open surgery, robot-assisted surgery reduced time spent in the hospital, reduced readmissions, and resulted in higher levels of fitness and quality of life; on all counts, this was demonstrated.
Professor John Kelly
“Despite robot-assisted surgery becoming more widely available, there has been no significant clinical evaluation of its overall benefit to patients’ recovery,” said Professor John Kelly, Professor of Uro-Oncology at UCL’s Division of Surgery & Interventional Science and consultant surgeon at University College London Hospitals. “In this study, we aimed to see if, as compared to open surgery, robot-assisted surgery reduced time spent in the hospital, reduced readmissions, and resulted in higher levels of fitness and quality of life; on all counts, this was demonstrated.”
“An unexpected discovery was the significant reduction in blood clots in patients getting robotic surgery; this indicates a safe surgery with far fewer problems, early mobilization, and a speedier return to normal life.”
“This is an important result,” said co-chief investigator Professor James Catto, Professor of Urological Surgery at the University of Sheffield’s Department of Oncology and Metabolism. When using this innovative surgery, patients spend less time in the hospital and recover faster.
“In the long run, this will relieve bed demands on the NHS and allow patients to return home sooner. We are seeing fewer issues as a result of greater mobility and less time spent in bed. The report also predicts future healthcare trends. We may soon be able to monitor recovery after discharge in order to identify people who are developing issues. It is feasible that tracking walking levels might identify people who require a district nurse visit or a hospital check-up sooner.”

“Previous trials of robotic surgery have focused on longer term outcomes. They have shown similar cancer cure rates and similar levels of long term recovery after surgery. None have looked at differences in the immediate days and weeks after surgery.”
Open surgery remains the NICE “gold standard” recommendation for highly complex surgeries, though the research team hope this could change.
“In light of the encouraging findings, the perception of open surgery as the gold standard for major surgeries is now being challenged for the first time,” Professor Kelly remarked. We expect that all qualified patients requiring major abdominal surgery will now be given the option of robotic surgery.”
“The Urology Foundation’s aim is straightforward,” stated Rebecca Porta, CEO of The Urology Foundation, “to save lives and decrease suffering caused by urological tumors and disorders.” We achieve this by investing in cutting-edge research, leading education, and supporting health care professional training to guarantee that fewer lives are lost.
“We are happy to have been at the forefront of a paradigm shift in the treatment and care of urology patients since our beginning 27 years ago, and the results of this experiment will improve the treatment and care of bladder cancer patients.”
Bladder cancer occurs when an abnormal growth of tissue, known as a tumor, develops in the bladder lining. The tumor may spread into the bladder muscle in some cases, leading to secondary cancer in other regions of the body. Every year, over 10,000 people in the UK are diagnosed with bladder cancer, and over 3,000 bladder ectomies and reconstructions are performed. It is one of the most costly cancers to treat.
Trial findings
338 patients with non-metastatic bladder cancer were randomly assigned to one of two groups in nine UK hospitals: 169 had robot-assisted radical cystectomy (bladder removal) with intracorporeal reconstruction (process of taking section of bowel to make new bladder), and 169 had open radical cystectomy.
The primary endpoint of the experiment was the length of stay in the hospital following surgery. The robot-assisted group stayed in the hospital for eight days on average, compared to ten days for the open surgery group – a 20% drop. Readmission to the hospital within 90 days of surgery was also dramatically reduced: 21% for the robot-assisted group vs 32% for the open group.
A total of 20 secondary outcomes were evaluated 90 days, six months, and twelve months after surgery. These factors included the prevalence of blood clots, wound complications, quality of life, disability, stamina, activity levels, and survival (morbidity). All secondary outcomes were better or almost equal to open surgery by robot-assisted surgery. Both robot-assisted and open surgery are equally successful in terms of cancer recurrence and length of survival, according to this and earlier research.
Following steps
The study team is carrying out a health economic analysis to calculate the quality-adjusted life year (QALY), which takes into account both the quantity and quality of life.