The human heart is the first organ to develop, and its development is fairly well documented. In theory, the heart can regenerate because its cardiomyocytes can divide and the adult heart contains a cardiac stem cell niche that can differentiate into cardiomyocytes and other cardiac-associated cell types. However, as with most other organs, these mechanisms are not activated in the event of serious injury.
Mechanical hearts stimulate regeneration in dormant parts of failing hearts, according to a UT Southwestern pilot study that shows promise for developing regenerative heart therapies.
“By all accounts, this is a small study, but it represents the first evidence that mechanical hearts, which are tried and true, approved treatments for patients with end-stage heart failure, can generate new muscle tissue in the failing human heart,” said lead author Hesham Sadek, M.D., Ph.D., Professor of Internal Medicine, Biophysics, and Molecular Biology.
His findings, which were published in the American Heart Association’s flagship journal Circulation, discovered that left ventricular assist devices (LVADs), which are widely accepted in cardiology as life-saving interventions, showed metabolic reactivation in myocardial areas with little or no activity.
This study discovered evidence of regeneration in parts of the heart that would normally be considered dead. It’s a promising finding that will prompt additional research to replicate the findings on a larger scale, and if confirmed, to investigate potential new therapies to amplify this process in the context of LVAD support.
Dr. Vlad Zaha
“What we need to do now is replicate these findings in larger studies,” said Dr. Sadek. “If these findings hold up in larger studies, mechanical hearts could emerge as a regenerative therapy to reverse heart failure, which is the holy grail in heart failure treatment.”
Dr. Sadek has made significant advances in this field of cardiology research, with studies of heart regeneration in mice published in the journals Nature and Science. Cell published his findings that oxygen metabolism damages DNA in heart cells, impairing their ability to regenerate. The study was co-led by Vlad Zaha, M.D., Ph.D., Assistant Professor of Internal Medicine, and Dr. Sadek.
“This study discovered evidence of regeneration in parts of the heart that would normally be considered dead,” Dr. Zaha explained. “It’s a promising finding that will prompt additional research to replicate the findings on a larger scale, and if confirmed, to investigate potential new therapies to amplify this process in the context of LVAD support.”
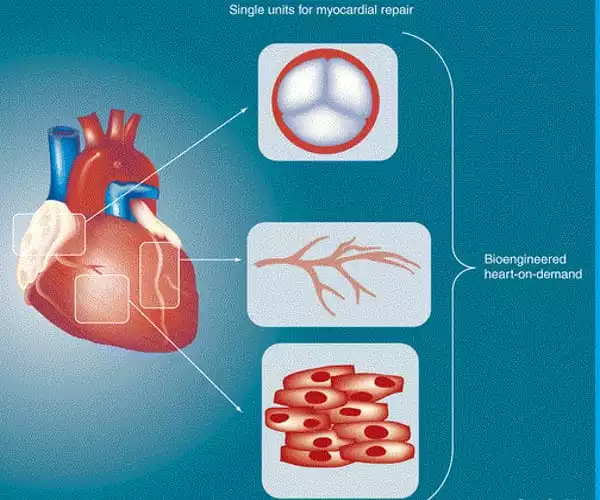
Human development begins with the fertilization of an ovum by a sperm, which triggers a frenzy of but intricately controlled cell division. At the time of implantation, the embryo is known as a blastocyst, and it is made up of an outer trophoblast and an inner cell mass made up of embryonic stem (ES) cells. These ES cells divide, move, respond to cues from themselves and each other, and exhibit pluripotency, or the ability to develop into all of the human body’s tissues and organs.
As the embryo develops into a foetus, the cells lose their pluripotency and become more differentiated, assisting in the formation of organs. As a result, their potency becomes increasingly limited. Every organ and tissue in the adult body contains a niche of stem cells, the potency of which is generally limited to the cells of the resident tissue.
The heart is the first organ to form in the developing embryo. The vertebrate heart develops from two regions of splanchnic mesoderm, one on each side of the developing embryo, that interact with the directly adjacent tissue, the anterior endoderm. The presence of the anterior endoderm is required for heart development, and the interaction between these two tissues results in the specification of cells destined to form the heart – the cardiogenic mesoderm.
The pilot study of four patients, ages 39 to 59, taking heart failure medications, measured metabolic activity by tracking a radiolabeled sugar molecule called F-fluorodeoxyglucose (FDG) in the heart. This FDG signal is thought to be a marker of “viable,” or alive, heart tissue.
FDG uptake was tracked using positron emission tomography (PET) imaging every six months for up to 18 months. At baseline, all participants had some degree of increase in FDG uptake in areas of previous metabolic inactivity, indicating possible myocardial regeneration. The increase in FDG uptake from baseline ranged from 1.87 percent to 23.80 percent among the four patients.