Tiny molecules in breast milk may protect infants from developing allergies. Breast milk contains various components that are known to boost the immune system and protect against infections. One of these components is called human milk oligosaccharides (HMOs), which are complex sugar molecules that cannot be digested by infants but are instead consumed by beneficial bacteria in the gut.
According to a new study, small molecules found in most human breast milk may reduce the risk of infants developing allergic conditions such as atopic dermatitis and food allergies.
Breastfed babies are thought to have fewer allergic conditions, such as eczema and food allergies, than formula-fed babies; however, the reason for this is unknown. According to a new study from Penn State College of Medicine, small molecules found in most human breast milk may reduce the likelihood of infants developing allergic conditions such as atopic dermatitis and food allergies. The discovery, according to the researchers, could lead to strategies for mothers, such as encouragement and support for breastfeeding or dietary and exercise interventions, to help reduce the likelihood of their babies developing allergies.
Atopic conditions, such as food allergies, asthma, and a skin condition known as atopic dermatitis, affect approximately one-third of children as a result of inappropriate immune system activation in response to environmental exposures.
There are nearly 1,000 different kinds of miRNAs in human breast milk, and their composition varies depending on maternal characteristics such as weight, diet, and genetics. Based on previous research showing relationships between these miRNAs and certain allergic conditions, we hypothesized that four of these miRNAs could have a protective effect against infant allergies.
Dr. Steven Hicks
“We don’t fully understand the biology behind this, but infants who breastfeed beyond three months may have a lower risk for these conditions,” said Dr. Steven Hicks, associate professor of pediatrics and pediatrician at Penn State Health Children’s Hospital.
Hicks’ research is concerned with the interaction of the environment, biology, and neurodevelopment and growth in children. His previous research shows how micro ribonucleic acids (miRNAs), tiny molecules that regulate gene expression throughout the body, can be used to diagnose conditions such as concussion or autism.
“There are nearly 1,000 different kinds of miRNAs in human breast milk, and their composition varies depending on maternal characteristics such as weight, diet, and genetics,” Hicks explained. “Based on previous research showing relationships between these miRNAs and certain allergic conditions, we hypothesized that four of these miRNAs could have a protective effect against infant allergies.”

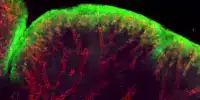
The researchers followed 163 mothers who planned to breastfeed for at least four months and their infants from birth through 12 months. They tracked how long each baby breastfed, and measured the miRNA composition of each mother’s breast milk over the course of lactation (0, 4 and 16 weeks). The team calculated the amount of specific miRNAs infants consumed based on reported breastfeeding patterns and the concentration of certain miRNAs in mothers’ milk samples. The researchers evaluated infants for atopic dermatitis, food allergies and wheezing throughout the study.
Of the infants studied, 41 (25%) developed atopic dermatitis, 33 (20%) developed a food allergy, and 10 (6%) developed wheezing. Infants who did not develop atopy consumed more miRNA-375-3p (miR-375) in their mothers’ breastmilk than infants who did. There were no other differences in maternal traits, infant traits, or environmental exposures between infants with atopy and infants without atopy. The researchers also discovered that levels of this miRNA increased throughout lactation and that mothers with a lower BMI had a higher concentration of miR-375. The findings were published in The American Journal of Clinical Nutrition.
“The fact that miR-375 content increased during lactation may explain why sustained breastfeeding has been linked to lower atopy in some studies,” Hicks said. He observed that the highest increase in miR-375 occurred in the first month after birth, but that the trend continued between months one and four. “Unlike formula, which does not contain human miRNAs, miR-375 is found in more than 99% of human milk samples and accounts for less than 1% of all miRNAs in breastmilk.”
According to Hicks, the study’s findings could lead to new interventions to help prevent infant allergies. Future research will concentrate on confirming these findings, defining the mechanisms by which miR-375 prevents allergies, and investigating interventions to increase miR-375 levels in maternal breast milk. Hicks also stated that with more research, miR-375 could one day be added to formula, which currently does not contain any miRNAs, to help address the fact that formula-fed babies are more likely to develop atopic conditions.