A new clinical experiment reveals that the medicine vorinostat, combined with immunotherapy, can entice HIV-infected cells out of latency and assault them. The findings illustrate how close — yet still distant — researchers have come to establishing an HIV-1 cure.
Antiretroviral therapy (ART) prevent HIV replication, allowing HIV patients to lead relatively normal lives. Despite these treatments, some HIV remains dormant inside cells, a condition known as “latency.” If ART is interrupted, HIV will reactivate, begin to replicate, and produce acquired immunodeficiency syndrome (AIDS). To develop a cure, researchers have attempted to push HIV out of latency and target it for destruction.
A new clinical trial led by Cynthia Gay, MD, MPH, associate professor of infectious diseases, David Margolis, MD, the Sarah Kenan Distinguished Professor of Medicine, Microbiology & Immunology, and Epidemiology, and other clinicians and researchers at the UNC School of Medicine suggests that a combination of the drug vorinostat and immunotherapy can coax HIV-infected cells out of latency and attack them.
A team lead by Catherine Bollard, MD, from George Washington University supplied the immunotherapy, which involved taking white blood cells from trial participants and expanding them in the laboratory to increase the cells’ ability to target HIV-infected cells before re-infusing them at UNC. Their findings, published in the Journal of Infectious Diseases, revealed a minor dent in the latent reservoir, indicating that more work has to be done in the field.
This is not the result we wanted, but it is research that needed to be done. We are working on improving both latency reversal and clearance of infected cells, and we hope to do more studies as soon as we can, using newer and better approaches.
David Margolis
“We did show that this approach can reduce the reservoir, but the reductions were not nearly large enough, and statistically speaking were what we call a “trend” but not highly statistically significant,” said David Margolis, MD, director of the HIV Cure Center and senior author on the paper. “We need to create better approaches to flush out the virus and attack it when it comes out. We need to keep chipping away at the reservoir until there’s nothing there.”
DNA inside cell nuclei is kept in a tightly packed space by chromosomes, which act as highly organized storage facilities. When you unfurl a chromosome, you’ll find loop-de-loop-like fibers called chromatin. If you keep unfurling, you’ll see long strands of DNA wrapped around scaffold proteins known as histones, like beads on a string. Finally, when the unfurling is complete, you will see the iconic DNA double helix.
Vorinostat works by inhibiting a lock-like enzyme called histone deacetylase. By stopping this mechanism, tiny doors within the chromatin fibers unlock and open up, effectively “waking up” latent HIV from its slumber and making it vulnerable to an immune system attack. As a result, a tiny blip of HIV expression shows up on very sensitive molecular assays.
But the effects of vorinostat are short lived, only lasting a day per dose. For this reason, Margolis and other researchers are trying to find safe and effective ways to administer the drug and keep the chromatin channels open for longer periods of time. For the study, six participants were given multiple doses of vorinostat. Researchers then extracted immune cells from the participants and expanded the cells that knew how to attack HIV-infected cells.
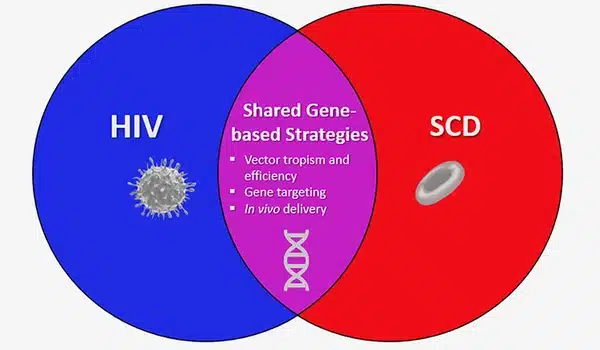
This immunotherapy method, which has been successful against other viruses such as Epstein-Barr virus and cytomegalovirus, involves returning participants’ expanded immune cells in the hopes that these cells will multiply even more and launch an all-out attack on newly exposed HIV-infected cells.
However, just one of the six patients experienced a decrease in their HIV reservoir levels throughout the first phase of the trial. To determine if the outcome was merely random or something more, researchers gave three subjects their usual dose of vorinostat while injecting five times the amount of customized immune cells. All three subjects had a modest drop in their reservoirs. However, the results were not statistically significant enough to be conclusive.
“This is not the result we wanted, but it is research that needed to be done,” said Margolis. “We are working on improving both latency reversal and clearance of infected cells, and we hope to do more studies as soon as we can, using newer and better approaches.”
Many of the study’s participants have been working with Margolis’ research team for years, devoting their own time and blood for research purposes. Their long-term relationship and commitment have been critical to data collection. The data, which shows the magnitude of the viral reservoir in these persons throughout the years preceding our study, makes the tiny alterations discovered more appealing.
“People living with HIV come in a couple of times a year, and we measure residual traces of virus in their blood cells, which doesn’t have any immediate benefit to them,” Margolis said. “It’s a very altruistic action and we couldn’t make any progress without their help.”