Gene therapy has emerged as a promising area of medical research, with the potential to treat a wide range of genetic disorders and diseases. While the typical approach to combating obesity involves lifestyle changes such as diet and exercise, researchers have looked into the potential of gene therapy as a novel strategy to combat obesity.
A scientific team from the University of Barcelona and the CIBERobn developed a strategy to combat obesity and diabetes in mice using ex vivo gene therapy, which involves implanting cells that have been manipulated and transformed to treat a disease. This is the first study to use ex vivo gene therapy to generate and implant cells expressing the CPT1AM protein, an enzyme that is important in many metabolic diseases such as obesity.
Professor Laura Herrero of the Faculty of Pharmacy and Food Sciences and the Institute of Biomedicine of the University of Barcelona (IBUB), as well as the Physiopathology of Obesity and Nutrition Networking Biomedical Research Centre (CIBERobn), led the study, which was published in the journal Metabolic Engineering.
Cell therapy is the process of introducing new cells into a tissue to combat disease. Cell therapies are currently being developed to treat hereditary diseases, both with and without the assistance of gene therapy, as well as degenerative diseases.
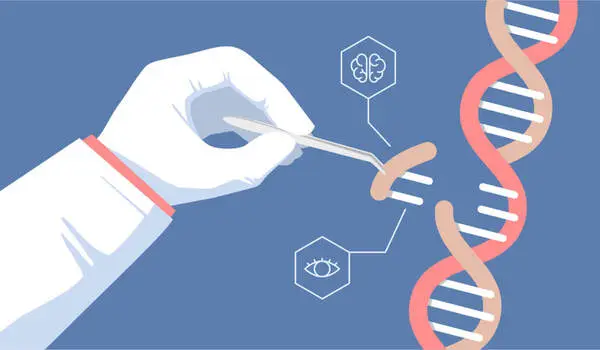
In this new therapy, animal models have been implanted subcutaneously with stem cells derived from adipose tissue, differentiated into adipocytes, so that they can express an active form of the CPT1AM protein, an enzyme located in the mitochondria that is key in lipid oxidation and is related to metabolic diseases.
Laura Herrero
“In this new therapy, animal models have been implanted subcutaneously with stem cells derived from adipose tissue, differentiated into adipocytes, so that they can express an active form of the CPT1AM protein, an enzyme located in the mitochondria that is key in lipid oxidation and is related to metabolic diseases,” explains Laura Herrero, a member of the UB Department of Biochemistry and Physiology.
“As a result, it was possible to reduce weight, fatty liver (hepatic steatosis), cholesterol, and glucose levels in obese mice.” Finally, implantation of adipocytes expressing the mitochondrial enzyme CPT1AM aids in the reduction of obesity and glucose intolerance in mice.”
As the cell transformation process takes place outside the body of the organism, this type of therapy is much easier to carry out and allows for greater control of the altered cells.
Obesity and cell therapy
Obesity and related metabolic disorders are a global health and social problem, which necessitates the development of novel therapeutic approaches. Adipose tissue is important in regulating energy balance, and adipose-derived mesenchymal stem cells (self-renewing cells) have gained interest in cell therapy.
CPT1A (carnitine palmitoyltransferase 1A) is the enzyme that regulates mitochondrial fatty acid oxidation. Our goal was to create adipocytes that could express a constitutively active form of CPT1A called CPT1AM, which could burn excess fat and improve mice’s obese metabolic phenotype after implantation.”
The new study’s findings support the future clinical application of this ex vivo gene therapy approach as a new strategy for lowering obesity and cholesterol rates in the population. This preclinical study could pave the way for future therapeutic strategies to combat obesity, which is currently a global health issue.
“To approximate the therapy in humans, we need to optimise several processes, such as the quality and viability of stem cells isolated from adipose tissue from people with obesity, the percentage of infection with lentivirus, and the number of cells used for transplantation,” researcher Laura Herrero concludes.