This study builds on decades of research demonstrating that the protein IL-24 has a broad anti-cancer effect, and it is the first to deliver the protein using T cells. This approach differs from CAR-T cells, which are designed to recognize proteins on the surface of cancer cells but have yet to be effective against solid tumors. Following treatment with IL-24 T cells, mice with prostate cancer experienced shrinkage of the primary tumor as well as distant metastases.
The study builds on decades of research by study co-senior author Paul B. Fisher, M.Ph., Ph.D., a member of Massey’s Cancer Biology research program, who discovered a protein called IL-24 that attacks cancer in a variety of ways.
Fisher collaborated with his colleague Xiang-Yang (Shawn) Wang, Ph.D., who co-directs the Developmental Therapeutics research program at Massey, to deliver the gene coding for IL-24, known as MDA-7, to solid tumors using T cells in this latest study.
Through T cell engineering, researchers at Virginia Commonwealth University Massey Cancer Center show that it’s possible to arrest tumor growth for a variety of cancers and squash the spread of cancer to other tissues.
“I think the beauty of what we’ve been involved in is that it broadens the scope of immunotherapy,” said Fisher, who is also the director of the VCU Institute of Molecular Medicine (VIMM) and the Thelma Newmeyer Corman Endowed Chair in Oncology Research at VCU. “Our approach is less reliant on cancer cells expressing a specific target.”
After all, this isn’t the first time T cells have been genetically modified to aid in cancer immunotherapy. The FDA-approved chimeric antigen receptor T (CAR-T) cell therapy has shown tremendous success in treating advanced cancers of the blood and lymphatic systems.
However, CAR-T has made limited progress in solid tumors such as prostate cancer and melanoma because the cells that make up those tumors aren’t all the same, preventing the engineered T cells from recognizing and attacking.
Wang and Fisher armed T cells with MDA-7/IL-24 to target cancer more broadly.
“Engineering T cells to produce MDA-7/IL-24 allows cancer cells to be killed regardless of target molecule expression. This will aid in the prevention of cancer cells evading immune attack “Wang is also a VCU professor of human and molecular genetics, the VIMM’s associate director of immunology, and the Harry and Judy Wason Distinguished Professor at Massey.
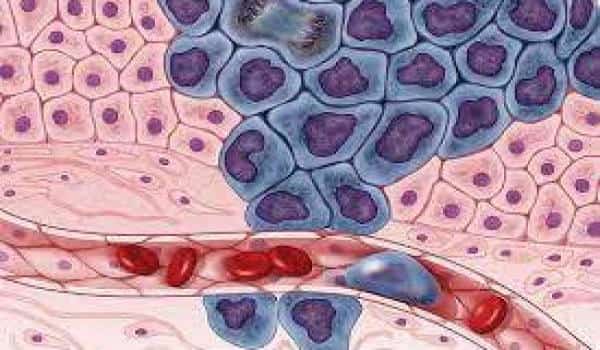
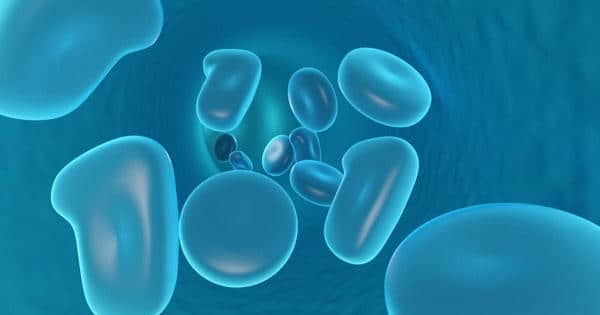
MDA-7/IL-24 binds to receptors on the surface of cells, instructing them to make and release more copies of the MDA-7/IL-24 protein. If the cell is healthy, the protein is simply secreted and no harm is done. However, if the cell is cancerous, MDA-7/IL-24 causes oxidative stress damage and, eventually, cell death, not only within the primary tumor but also among its distant metastases, which is the cause of death in 90% of patients.
As a result of this process, the immune system generates memory T cells that can theoretically kill the tumor if it ever comes back. At the whole tumor level, IL-24 also blocks blood vessel formation, starving tumors of the nutrients so badly needed to sustain their unchecked growth.
As a result of this process, the immune system produces memory T cells that, in theory, can kill the tumor if it recurs. IL-24 also inhibits blood vessel formation at the tumor level, depriving tumors of the nutrients they require to continue their unchecked growth.
In the clinic, this method would entail extracting the patient’s own T cells from tumor samples, genetically engineering them to express MDA-7/IL-24, growing millions of copies of the cells in the lab, and then transplanting them back into the patient. The procedure is generally safe and minimally invasive due to federally mandated manufacturing standards. MDA-7/IL-24 expression in CAR-T cells could also be engineered.
MDA-7/IL-24 T cells would most likely be used in conjunction with other therapies to be most effective. Although moving technology from the bench to the bedside is never easy, Fisher believes that much of the groundwork has already been done.
Several cancers are already undergoing clinical trials using various methods of delivering IL-24. A phase 1 trial that used an adenovirus, which is similar to the common cold, to deliver MDA-7/IL24 to the tumor demonstrated 44 percent efficacy against multiple types of cancer and was generally non-toxic.
“I believe we have a head start and a running ramp that could be significantly accelerated,” Fisher said.
Wang and Fisher recently received a National Cancer Institute grant to optimize their technology for the treatment of solid tumors and cancer metastases in preparation for future human trials.