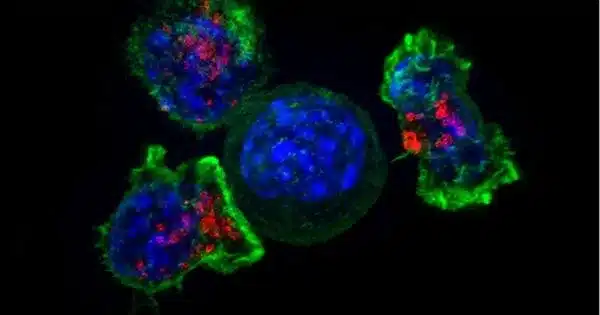
T lymphocytes, also known as T cells, are a type of white blood cell that plays an important role in the immune system. They help recognize and attack foreign substances like viruses, bacteria, and cancer cells.
Scientists discover an auto-signaling mechanism that drives the T cell anti-tumor response; findings could lead to new cancer therapies and biomarkers. When it comes to motivation, it is often necessary to look within. According to new research, cancer-fighting immune cells have discovered a way to do just that.
Scientists at the University of California San Diego have discovered a property of T cells that could inspire new anti-tumor therapeutics. Through a previously undescribed form of cell auto-signaling, T cells were shown to activate themselves in peripheral tissues, fueling their ability to attack tumors.
The study, published in Immunity, was led by study first author and postdoctoral fellow Yunlong Zhao, Ph.D., and co-senior authors Enfu Hui, Ph.D., professor in the School of Biological Sciences at UC San Diego, and Jack D. Bui, MD, Ph.D., professor of pathology at UC San Diego School of Medicine.
We discovered that local membrane curvatures are a rich dimension of T cell auto-signaling, which is a paradigm shift in a field that previously assumed this only occurred across cells.
Enfu Hui
T cells are a type of white blood cell that helps fight cancer and protects against infection. T cells are trained in the lymph organs by antigen-presenting cells, which, as the name implies, present an antigen (a piece of tumor or pathogen) to T cells, stimulating an immune response.
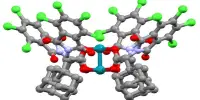
The binding of B7, a protein on the surface of antigen-presenting cells, with CD28, a receptor on T cells, is an important part of this process. This interaction between B7 and CD28 is a key driver of the T cell immune response. T cells that have been trained leave the lymph organs and travel throughout the body to find and attack their targets.
More recent work has since revealed that T cells can actually produce their own B7 or take the B7 protein from the antigen-presenting cells and bring it along with them, but exactly why they do this has remained unclear. This also led the researchers to wonder whether T cells, now equipped with both a receptor and its ligand, might be able to activate themselves.
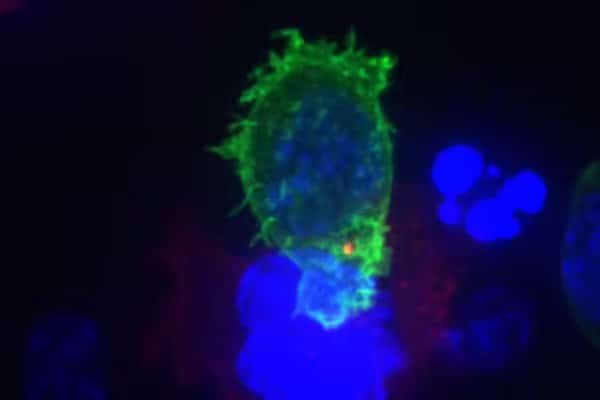
The researchers discovered that T cells can self-activate by puckering their cell membrane inwards, allowing the B7 protein and the CD28 receptor to bind to each other.
“People often assume the cell membrane is flat, but it actually looks more like a coastline with lots of coves and bays,” Hui explained. “We discovered that local membrane curvatures are a rich dimension of T cell auto-signaling, which is a paradigm shift in a field that previously assumed this only occurred across cells.”
The researchers then confirmed that the auto-stimulation was effective in increasing T cell function and slowing tumor growth in a cancer mouse model.
“When a T cell exits a lymph organ and enters a tumor environment, it’s like leaving home and going for a long trek in the woods,” said Bui. “The same way a hiker brings snacks to sustain them through the trip, the T cells bring their own signal to keep them going. Now the exciting question is, how much farther will they go if we can provide more food?”
Refueling the T cells could be achieved by either providing more sources of B7 in the lymph organs or in the tumor itself. Another option, the authors say, would be to develop a cell therapy in which engineered T cells with enhanced auto-signaling capabilities were delivered directly to a patient.
The researchers also propose that this system could be used as a cancer biomarker, with patients whose tumors contain a high number of T cells with B7 faring better against the disease. In patients with autoimmune diseases such as lupus or multiple sclerosis, on the other hand, physicians could prescribe endocytosis inhibitors to prevent the cell from forming concavities, effectively blocking the B7:CD28 interaction and reducing overactive T cell function.
“We’ve discovered a way for T cells to survive outside of their normal homes in the foreign environment of a tumor, and we can now develop clinical strategies for increasing or decreasing these pathways to treat disease,” Hui said.