A significant step forward has been made in the search for a treatment for the common diabetes complication hypoglycemia, or low blood sugar. Researchers discovered a method to help protect against hypoglycemia by boosting hormonal defense systems. The researchers believe they have discovered a promising target in the brain that could be used in future drug development to create an anti-hypoglycemia drug.
Blood sugar levels rise in all types of diabetes because the body is either unable to produce insulin, cannot produce enough of it, or the insulin produced is ineffective. This means that people with diabetes must manage their own blood sugar levels, which can frequently become dangerously high (hyperglycemia) or dangerously low (hypoglycemia) (hypoglycaemia).
Hypoglycemia, also known as “hypos,” frequently occurs at night, disrupting sleep and occasionally causing seizures. Anxiety, palpitations, sweating, and hunger are all symptoms of hypoglycemia. They can also cause dizziness, confusion, loss of consciousness, and, if left untreated, coma and even death.
Now, a study published in Frontiers in Endocrinology by the University of Exeter in collaboration with Rigel Pharmaceuticals has discovered a way to help defend against hypoglycemia by boosting hormonal defense systems. The researchers believe they have discovered a promising target in the brain that could be used in future drug development to create an anti-hypoglycemia drug.
Our findings suggest that activating the brain fuel gauge we discovered could be beneficial in preventing hypoglycemia. In the long run, we hope to develop a pill that can be taken before bed to prevent nighttime hypos.
Dr Craig Beall
The JDRF-funded and Diabetes UK-supported researchers conducted laboratory experiments with a pre-clinical test compound (R481) that acts similarly to metformin, a widely used type 2 diabetes drug. R481, on the other hand, works differently because it enters the brain and activates an important brain fuel gauge known as AMPK (AMP-activated protein kinase).
Dr Ana Cruz of the University of Exeter, the study’s lead author, stated: “Our findings emphasize the importance of better understanding brain-pancreas communication in order to strengthen the body’s defenses against hypoglycemia. I see the emotional and physical effects of hypoglycemia on a daily basis, and I believe that these findings have moved us one step closer to identifying targets within this brain-pancreas network to mitigate the effects of hypoglycemia.”
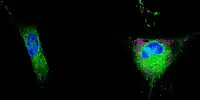
The researchers tested the compound on specialized brain glucose-sensing neurons (GT1-7 cells) in petri dishes and discovered that it works by activating this brain fuel gauge. They discovered that the drug boosts the hormonal defense against hypoglycemia in healthy rats by increasing the release of a hormone called glucagon from the pancreas. The drug activated a brain-pancreas link to protect against hypoglycemia, but it had no effect on fasting blood sugar levels.

Dr Craig Beall, senior study author from the University of Exeter, stated: “Our findings suggest that activating the brain fuel gauge we discovered could be beneficial in preventing hypoglycemia. In the long run, we hope to develop a pill that can be taken before bed to prevent nighttime hypos. This is only the first step on a long road, and we hope that one day we will be able to give people with diabetes and parents of children with diabetes some peace of mind that they will not have a bad nighttime hypo.”
“This early stage research, funded by Diabetes UK, has uncovered important links between the brain and the pancreas, which could lead to new treatments to help people with diabetes avoid hypos or restore their ability to recognize signs of low blood sugars,” said Dr Lucy Chambers, Head of Research Communications at Diabetes UK, which supported the study.
“Hypos and hypoawareness can be dangerous and debilitating, and they can have a significant impact on the daily lives of people with diabetes of all types. New treatments for hypos, or hypoawareness, would make living with diabetes much easier, reducing anxiety and, most importantly, protecting people from the serious consequences that hypos can have.”
According to Conor McKeever, Research Communications Manager at the type 1 diabetes charity JDRF: “People with type 1 diabetes report that hypoglycemia is one of the things they fear the most about their condition, so a treatment to prevent hypos would go a long way toward alleviating some of the burden that comes with living with type 1. It may also help to alleviate the anxiety felt by family members, who tell us they frequently lose sleep because they are afraid their loved one will have a hypo in the middle of the night. We are proud to have funded this research and are excited to see how it progresses toward a new treatment for the 400,000 people in the UK who have type 1 diabetes.”
Evidence suggests that the 400,000 people in the UK with type 1 diabetes have two episodes of hypoglycemia per week, with one severe episode per year. Hypoglycemia can occur up to five times per year in people with type 2 diabetes. Although the frequency of type 2 diabetes is lower, the overall rate is higher because the condition affects well over 4 million people in the United Kingdom.
The structure of the compounds was published in the paper ‘Brain permeable AMP-activated protein kinase activator R481 raises glycemia by autonomic nervous system activation and amplifies the counter regulatory response to hypoglycemia in rats.’ It was published in the journal Frontiers in Endocrinology.