Researchers found Treatment Shows promising results in Heart Failure after Myocardial Infarction
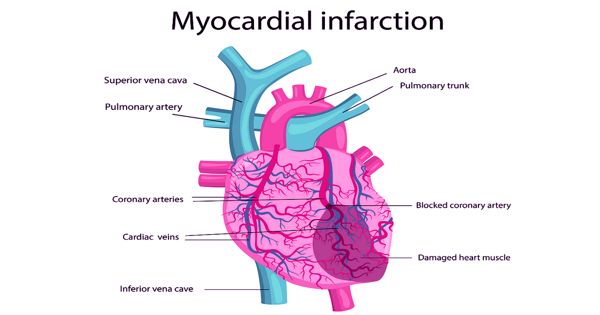
Myocardial infarction is a common cause of heart failure (HF), which can develop soon after AMI and may persist or resolve or develop late. While there are therapies to aid in overall heart health, there are very few preventative therapies for heart failure after a significant heart attack, a serious condition that has very significant mortality. Heart failure (HF) is a common complication of myocardial infarction (MI), which may develop early or late and persist, resolve or recur. However, researchers at Baylor College of Medicine have found a potential treatment that has shown promising results in mice.
Understanding the drivers of morbidity and mortality after MI is important, given the great difference in mortality rates reported in clinical trials of MI compared to epidemiological studies. The findings, published in the latest edition of the Proceedings of the National Academy of Sciences, showed that stimulation of a steroid receptor coactivator, SRC-3, by a molecule known as MCB-613 after a heart attack prevented the scar and maladaptive repair of heart tissue that can lead to heart failure. Improved understanding about which patients are at risk and the nature of the risk could help focus attention on patients at greater need, to ensure that they receive appropriate therapy.
Heart failure (HF) is a common complication of myocardial infarction (MI), which may develop early or late and persist, resolve or recur. However, researchers at Baylor College of Medicine have found a potential treatment that has shown promising results in mice.
Treatment can only help patients who are at risk of complications that the treatment aims to prevent. “Heart failure after a significant heart attack is a leading cause of death in humans. It often occurs over a few years; a person becomes weaker and weaker and eventually they die,” said Dr. Bert O’Malley, professor of molecular and cellular biology at Baylor and lead author of the study. “In the mouse model, our team has been able to show that MCB-613 decreases damaging remodeling when given within hours after a myocardial infarction, thereby inhibiting the subsequent development of heart failure.”
The optimal management of the patient with HF complicating MI varies according to time since the onset of infarction. Researchers had previously discovered and characterized MCB-613 as a small molecule stimulator for SRCs. The family of SRCs is responsible for cellular plasticity and cell growth pathways during both normal and abnormal tissue growth. After a heart attack, the damaged tissue scars. This results in tissue loss and increased inflammation, fibrosis, and a progressive decrease in cardiac function, all of which are hallmarks of myocardial infarction-induced heart failure. Cardiogenic shock is an extreme presentation of HF after MI and is a leading cause of death in the MI setting. The only therapy proven to reduce mortality for patients with cardiogenic shock is early revascularization.
The molecule works by stimulating SRC-3, thus initiating a complex cascade of events in tissue repair and modulation of the inflammatory response. O’Malley and his team also found that after treating the mice model with MCB-613, there were no significant signs of toxicity.
“Our findings show us that this molecule acts directly on heart tissue repair and regeneration after a severe heart attack; however, more studies are needed to fully understand the safety and efficacy before we are able to use this as a therapy in humans,” O’Malley said
Several studies are examining new approaches to mitigate the occurrence and adverse impact of post-MI HF. These studies are testing drugs for HF and diabetes and are evaluating mechanical support devices to bridge patients to recovery or transplantation. “Our study shows promise to address the unmet need for treatments to prevent damage to heart tissue following a heart attack. These findings pave the way for the discovery of additional treatments to target chronic heart disease progression,” said Dr. Lisa Mullany, assistant professor of molecular and cellular biology and first author on the study.
Heart failure is a devastating disease that is more lethal than all cancers combined, and currently, there are no definitive therapies other than heart transplantation. Clinically, forward failure of the heart leads to low blood pressure and fatigue, while backward failure results in dyspnea and fluid retention, which may lead to pulmonary congestion, pleural effusions, and peripheral edema, as well as impairment of hepatic, gastric, and renal function.