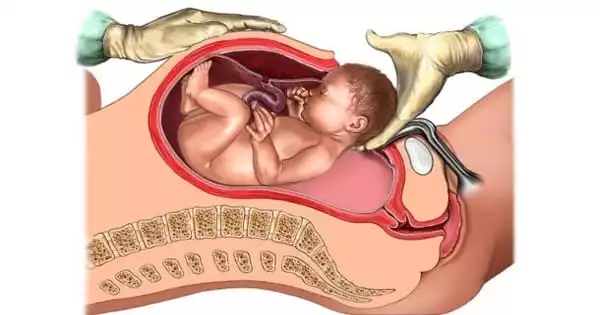
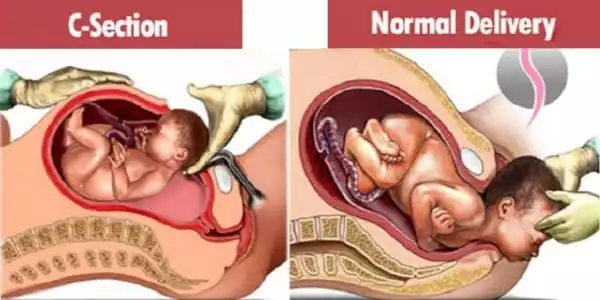
The birth of a child is, without a doubt, the most joyous event in most people’s lives, yet childbirth does not always go as planned in the family. The majority of women prefer to give birth normally, and only a handful are prepared for a caesarean section. When delivery is naturally dangerous to the woman, the fetus, or both, a Caesarean section is recommended. It is also advised in the presence of contraindications to vaginal birth when such conditions emerge in pregnancy or during childbirth that the pregnancy must be completed as soon as possible and vaginal delivery is not possible or appropriate. An emergency caesarean section is sometimes needed to prevent health complications for the mother or for the baby or to save the life of the mother and baby.
Caesarean delivery (CD) is a surgical operation used when a vaginal delivery (VD) may endanger the baby or the mother. The prevalence of CD has risen considerably during the last few decades. The CD rate in the United States has risen from 5.8 percent in 1970 to 32.3 percent in 2008. Similarly, it has been quickly expanding in developing countries since the 1980s. According to the WHO report, the overall rate of CD in Asia in 2007–2008 was 27.3 percent, with China having the highest rate of 46.2 percent, and 40 percent of cesareans reported to have no clinical grounds.
If a pregnant woman experiences aberrant conditions during vaginal delivery, an emergency cesarean section (EmCS) can be a life-saving treatment. EmCS is a difficult process that occurs only under specific obstetric situations and necessitates awareness and timely assessment of the risky scenario.
In births where labor is involved, there is more inflammatory gene expression in the placenta if you had an emergency Caesarean section compared to vaginal birth. This study also indicates that babies, in particular females, could be more compromised in their development and long-term health and wellbeing after an emergency C-section.
Dr. Anya Arthurs
Labor and natural childbirth put a strain on a mother’s body, but an emergency Caesarean section is linked to even higher inflammatory gene expression in the placenta, according to new South Australian research.
The study, led by Flinders University’s Pregnancy Health and Beyond (PHaB) Lab and other researchers, looked at differences in placenta inflammation markers after delivery of both male and female babies who had 20 emergency Caesarean procedures compared to 40 vaginal (or ‘natural’) deliveries and 10 elective C-sections at an Adelaide public maternity hospital between 2006 and 2018.
“Because labor is an inherently inflammatory process, having a planned or pre-labor Caesarean section will result in less inflammasome activation than having an emergency C-section in a woman who is already in labor or having an unassisted vaginal birth,” explains Dr. Anya Arthurs, the lead author of a new article published in Frontiers of Immunology.
“In births where labor is involved, there is more inflammatory gene expression in the placenta if you had an emergency Caesarean section compared to vaginal birth. This study also indicates that babies, in particular females, could be more compromised in their development and long-term health and wellbeing after an emergency C-section.”
“Importantly, while placentas tested from baby boys have more inflammatory gene expression from a vaginal or ‘natural’ birth, placentas tested from baby girls have more inflammatory markers,” says senior author Matthew Flinders Professor Claire Roberts of the Flinders Health and Medical Research Institute.
“One explanation could be our discovery that placentas from newborn boys emit ‘warning signals’ (known as ‘interleukin-33’) at times of fetal distress, which we did not notice in placentas from baby girls. This may assist to reduce the amount of inflammation.”
Overall, the measurement of inflammatory gene expression in the placenta could be used to identify newborns who have been exposed to higher-than-normal levels of inflammation at birth, creating incentives to closely monitor their development and long-term health and welfare, the researchers conclude.
In clinical situations, the information contained in the risk assessment system can be examined prior to delivery. As a result, this risk score system is straightforward, easy to use, and has good reproducibility in clinical practice. If the score is excessively high, we should pay great attention to the circumstances of moms, and newborns should be closely checked throughout childbirth.
The goal of this study is to thoroughly investigate 22 maternal and fetal parameters in terms of pregnant women’s demographics, pregnancy history, perinatal problems, neonatal features, and labor process in order to identify high-risk factors related to EmCS before delivery. The risk of EmCS during vaginal birth was then quantified using a risk score system.