A study funded by the National Institutes of Health discovered that moderate levels of two outdoor air pollutants, ozone, and fine particulate matter, are associated with non-viral asthma attacks in children and adolescents living in low-income urban areas. The study also discovers links between the two pollutants and molecular changes in the children’s airways during non-viral asthma attacks, implying possible mechanisms for those attacks.
According to the researchers, the observational study is one of the first to link elevated levels of specific outdoor air pollutants in specific urban locations to distinct changes in the airways during asthma attacks that are not caused by respiratory viruses. The findings were published in The Lancet Planetary Health today.
“The strong association this study demonstrates between specific air pollutants among children in impoverished urban communities and non-viral asthma attacks further augments the evidence that reducing air pollution would improve human health,” said Hugh Auchincloss, M.D., acting director of the National Institute of Allergy and Infectious Diseases (NIAID), part of NIH.
The study was conducted by the NIAID-funded Inner City Asthma Consortium under the leadership of Matthew C. Altman, M.D., M.Phil., and Daniel J. Jackson, M.D. Dr. Altman is an associate professor in the department of medicine at the University of Washington School of Medicine and an associate scientist at the Benaroya Research Institute at Virginia Mason in Seattle. Dr. Jackson is a professor of pediatrics and medicine in the School of Medicine and Public Health at the University of Wisconsin-Madison.
The strong association this study demonstrates between specific air pollutants among children in impoverished urban communities and non-viral asthma attacks further augments the evidence that reducing air pollution would improve human health.
Hugh Auchincloss
Asthma is caused by chronic inflammation of the airways. During an asthma attack, the airway lining swells, the muscles surrounding the airways contract, and the airways produce extra mucus, significantly narrowing the space for air to move in and out of the lungs. Children living in low-income urban areas in the United States are especially vulnerable to attack-prone asthma. Asthma attacks triggered by respiratory virus infections – a common trigger – have been extensively studied, but those that occur independently of such infections have not.
There are several specific outdoor air pollutants that have been linked to asthma attacks in urban children. These include:
- Ozone: This is a highly reactive gas that is formed when sunlight reacts with pollutants such as nitrogen oxides and volatile organic compounds (VOCs). Ozone can irritate the respiratory system and trigger asthma attacks.
- Fine particulate matter (PM2.5): This is a type of air pollution made up of tiny particles that are smaller than 2.5 micrometers in diameter. Fine particulate matter can be inhaled deep into the lungs and has been linked to asthma attacks in children.
- Nitrogen dioxide (NO2): This is a toxic gas that is produced by the burning of fossil fuels. It can irritate the respiratory system and trigger asthma attacks in children.
- Sulphur dioxide (SO2): This is a pungent gas that is produced by the burning of fossil fuels and other industrial processes. It can irritate the respiratory system and trigger asthma attacks in children.
- Carbon monoxide (CO): This is a colorless, odorless gas that is produced by the incomplete burning of fossil fuels. It can reduce the amount of oxygen in the blood and trigger asthma attacks in children.
It is important to note that children with asthma may also be sensitive to other outdoor air pollutants, such as allergens like pollen and mold spores.

The current study looked at the relationship between air pollutant levels and asthma attacks in the absence of a respiratory virus in 208 children aged 6 to 17 who had attack-prone asthma and lived in low-income neighborhoods in one of nine U.S. cities. The researchers then validated the associations they discovered between air pollutant levels and non-viral asthma attacks in an independent cohort of 189 children with persistent asthma aged 6 to 20 years who also lived in low-income neighborhoods in four U.S. cities.
The children were followed prospectively for up to two respiratory illnesses or six months, whichever came first. Each illness was classified as viral or non-viral, as well as whether or not it involved an asthma attack. The researchers matched each illness with the Environmental Protection Agency’s air quality index values and individual air pollutant levels in the relevant city on the dates surrounding the illness. The researchers then adjusted their data for city and season to reduce the impact of these variables on the results.
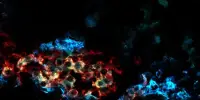
According to previous research, nearly 30% of children with asthma had a non-viral cause, which is two to three times the proportion seen in non-urban children. These attacks were linked to elevated levels of fine particulate matter and ozone in the surrounding air. By analyzing nasal cell samples obtained from children during respiratory illnesses, the researchers linked changes in the expression of specific sets of genes that play a role in airway inflammation to elevated levels of these two pollutants. Some of the identified gene-expression patterns suggest that non-viral asthma attacks may involve distinct biological pathways.
Given the findings of the study, it will be critical to develop and test various strategies to see if they can prevent or reduce pollution-related asthma attacks in urban children. Treatments designed to counteract the harmful effects of elevated levels of outdoor air pollutants on airway inflammatory responses linked to non-viral asthma attacks, as well as devices for personalized monitoring of local outdoor air pollutant levels to inform asthma management, may be included in these strategies.