Millions of people suffering from neurological and psychiatric illnesses such as trauma, addiction, and chronic pain are treatment-resistant. In fact, about 30 percent of all major patients with depression do not respond to either treatment or psychotherapy at all. Simply stated, certain conventional types of therapy may have hit their limit with these conditions. From here, where are we going? New research paves the way for a promising alternative: personalized deep brain stimulation.
Researchers have found a way to predict what effect electrical stimulation will have on an individual’s brain activity across multiple brain regions. The work represents a major step forward in achieving new therapies for a whole host of neurological and mental disorders.
Study to be published by the Andrew and Erna Viterbi Early Career Chair of Electrical and Computer Engineering at the USC Viterbi School of Engineering in Nature Biomedical Engineering, headed by Maryam Shanechi, paves the way for a potential alternative: personalized deep brain stimulation. For an entire host of neurological and behavioral illnesses, the study marks a big move forward toward achieving alternative treatments.
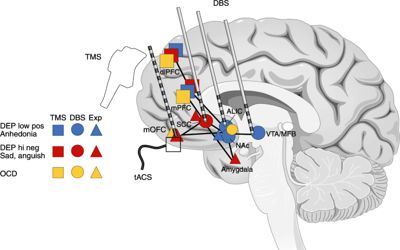
Direct electrical stimulation can modulate the operation of brain networks for the treatment of many neurological and neuropsychiatric diseases and for restoring impaired function. Precise neuromodulation, however, allows a person to precisely model and forecast the effects of stimulation on the operation of their large brain networks.
The human brain itself has been, until now, the problem of personalized deep brain stimulation. Mental illnesses can appear in the brain of each patient differently. Similarly, it can be somewhat different when and how the brain function of each patient and their symptoms can respond to stimuli. This makes it impossible to know the effect of stimulation in a given patient or how to adjust the dosage of stimulation over time to match it to the needs of a patient—that is, the amplitude or frequency.
By discovering experimental stimulus waveforms and constructing new machine-learning models, Shanechi and her team have found a way to determine what influence electrical stimulation can have on the brain activity of a person across different brain regions. In collaboration with Bijan Pesaran, Professor of Neural Sciences at NYU, they showed the model’s effectiveness in real brain stimulation studies.
They developed two instruments to achieve this: a novel electrical stimulus wave to map brain activity; and new machine-learning methods to learn the map from brain data obtained during stimulation. “Our wave, which changes its amplitude and frequency randomly in time, allowed us to see and predict how the brain responded to a wide range of stimulation doses,” Shanechi said. Much like any door can be opened by a skeleton key, the wave can be extended to the brain of any human and provide a personalized map of how it reacts to stimuli. The researchers applied their waves to four distinct areas of the brain to test their theory. In each case, they were able to predict the outcome of brain activity across multiple regions for the first time.
What this means is that, by adjusting the amplitude and frequency of stimulation, doctors can shortly be able to personalize a’ dosage’ of deep brain stimulation on a case-by-case basis and in real-time. Think of it as a version of brain stimulation to maximize or decrease the amount of milligrams in a pill. The effects are huge for persons suffering from psychiatric illnesses such as treatment-resistant depression or anxiety.
Machine learning strategies for interpreting signs of psychiatric conditions such as mood from brain function were previously developed by Shanechi and her colleagues. Today, with their new abilities to help assess how stimulus on an individual basis impacts brain function, they are trying to integrate their discoveries with customized behavioral illness treatments. “By putting these two boxes together, we hope to build closed loop brain-machine interfaces that adjust the dose of electrical stimulation therapy by tracking the symptoms in real-time based on brain activity and by predicting how a change in stimulation can change the activity and thus these symptoms,” Shanechi said.
















