Harvard researchers explain – Cells can be revived after Heart Attacks
Researchers have unraveled possible pathways behind the healing capacity of extracellular vesicles and shown their ability not only to regenerate cells during a heart attack but also to maintain cells functioning despite being deprived of oxygen during a heart attack. Researchers have shown this capability in human tissue by using an integrated heart-on-a-chip sensor that continuously tracks tissue contractions.
Researchers at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) have now unraveled possible pathways behind the therapeutic capacity of EVs and shown their ability not only to regenerate cells during a heart attack but to maintain cells functioning despite being depleted of oxygen during a heart attack.
Extracellular vesicles (EVs)-nanometer-sized messengers flying between cells to carry signals and cargo-are exciting instruments for the next generation of treatments for anything from autoimmune and neurodegenerative disorders to cancer and tissue injuries. Stem cell EVs have also been shown to aid the heart cells to heal from a heart attack, but it remains a mystery how they help and whether the beneficial result is unique to stem cell EVs.
Researchers at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) have now unraveled possible pathways behind the therapeutic capacity of EVs and shown their ability not only to regenerate cells during a heart attack but to maintain cells functioning despite being depleted of oxygen during a heart attack. Researchers have shown this capability in human tissue by using an integrated heart-on-a-chip sensor that continuously tracks tissue contractions.
The team also demonstrated that these intercellular travelers could be derived from endothelial cells, which line the surface of blood vessels and are more abundant and easier to maintain than stem cells.
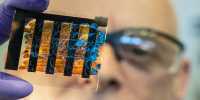
The study is published in the journal Science Translational Medicine. “Our organ-on-chip technology has progressed to the point where we can now fight drug targets instead of fighting the chip design,” said Kit Parker, Tarr Family Professor of Bioengineering and Applied Physics at SEAS and senior author of the report. “With this study, we have mimicked a human disease on a chip with human cells and developed a novel therapeutic approach to treat it.”
Heart problems, or myocardial infarctions, occur as the supply of blood to the heart is blocked. Of course, the easiest way to cure a heart attack is to restore blood supply, but this procedure will also do further harm to the heart cells. So-called ischemia-reperfusion injury (IRI) or reoxygenation injury occurs as the blood flow returns to the tissue following a period of oxygen deprivation.
This is where the endothelial-derived EVs (EEVs) come in. Since these vesicles are derived from vascular tissue, which is specifically tuned to feel hypoxic tension, the researchers speculated that the cargo they hold could provide direct safety to the heart muscle.
The researchers mapped the entire set of EEV proteins that are or can be, expressed by the vesicles. The team tested the effect of EEVs on human heart tissue using a heart-on-chip model developed by the SEAS Disease Biophysics Community. Organ-on-chip systems replicate the shape and function of native tissue and allow researchers to study the results of injury and treatment in human tissue in real-time. Here the researchers simulated a myocardial infarction and reoxygenation of the chips that were infused with EEVs and those that were not.
Researchers observed that cardiomyocytes could better respond to stress conditions and retain a higher workload in tissues treated with EEVs. The researchers caused damage by three hours of oxygen restriction followed by 90 minutes of reoxygenation and then assessed the fraction of dead cells and the contractile strength of the tissue. The cardiac tissue treated with EEVs had twice as many dead cells and had contractile strength four times greater than the untreated tissue after damage.
The team also observed that wounded cardiomyocytes treated with EEVs had a collection of proteins that were more similar to uninjured proteins relative to untreated cells. Surprisingly, the team also found that EEV-treated cells tended to contract even without oxygen.
“Our findings indicate that EEVs could protect cardiac tissue from reoxygenation injury in part by supplementing the injured cells with proteins and signaling molecules that support different metabolic processes, paving the way for new therapeutic approaches,” said André G. Kléber, Visiting Professor of Pathology at Harvard Medical School and co-author of the report.
The research was co-authored by Johan U. Lind, a former postdoctoral fellow at SEAS and current Assistant Professor at the University of Copenhagen, Denmark; Herdeline Ann M. Ardoña, a former postdoctoral fellow at SEAS and current Assistant Professor at the University of California Irvine; Sean P. Sheehy, Lauren E. Dickinson, Feyisayo Eweje, Maartje M.C. Bastings, Benjamin Pope, Blakely B. O’Connor, Juerg R. Straubhaar and Bogdan Budnik.