Controlled, localized delivery of blood thinners has the potential to improve blood clot treatment. Anticoagulants, or blood thinners, are commonly used to prevent and treat blood clots. Their systemic administration, on the other hand, carries risks, such as an increased risk of bleeding.
Researchers combined heparin with a protein fragment called a peptide to slow the drug’s release and deliver the medication directly to the site of a clot. Heparin has long been used as a blood thinner, or anticoagulant, to prevent complications in patients with blood clotting disorders or after surgery. However, the medication is still difficult to dose correctly, which could result in overdosing or underdosing.
A team of Penn State researchers combined heparin with a protein fragment, peptide, to slow down the release of the drug and convey the medication directly to the site of a clot. They published their findings in the journal Small.
We wanted to develop a material that can gradually deliver heparin over time rather than the current iteration that gets cleared from the body in a couple of hours. We also wanted to deliver the drug through the skin instead of through an IV.
Scott Medina
“We wanted to develop a material that can gradually deliver heparin over time rather than the current iteration that gets cleared from the body in a couple of hours,” said corresponding author Scott Medina, Penn State associate professor of biomedical engineering. “We also wanted to deliver the drug through the skin instead of through an IV.”
When positively charged peptides and negatively charged heparin are combined, they form a nanogranular paste that can be injected beneath the skin, forming a cache of material that is then diffused in the circulatory system and travels to blood clots as they form. The turbulent flow of fluid near a blood clot causes the two materials to separate, allowing heparin to start working as an anticoagulant.
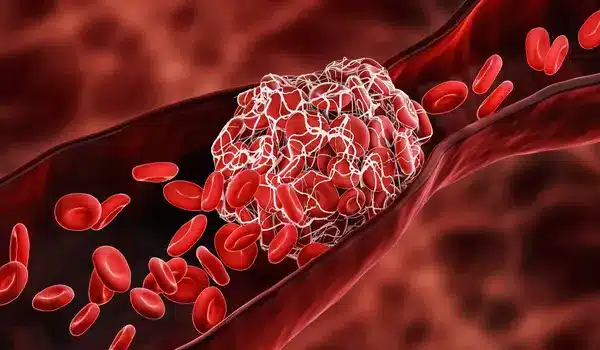
“The peptide is ideal for pairing with heparin because it essentially blocks heparin’s action until it is needed in the body,” said Atip Lawanprasert, first author on the paper and a doctoral student in biomedical engineering. “On its own, the peptide has some anticoagulant properties: it binds to platelets in the blood, allowing action at the clotting site.”
Heparin’s anti-clotting properties are applied indiscriminately, not just at blood clot sites, and it clears quickly, with a half-life of 60 to 90 minutes. Using preclinical animal trials, researchers discovered that the addition of peptide extends the half-life of heparin to nearly 24 hours.
“The peptide extends the effects of heparin more than ten times longer than what is currently used,” Medina said. “The longer half-life allows for longer treatments for patients, less medication waste, and more precise dosing.” Eventually, instead of an all-day IV drip, the medication could be injected under the skin just once a day.”
Following that, the researchers intend to replicate the study in a clinical setting, as well as investigate the effect of the medication’s toxicity in the body if administered over multiple days.
















