Abnormal heart rhythms (arrhythmias) are patterns of heartbeats that are erratic, too fast, too slow or are performed through an abnormal electrical pathway through the heart. About 300,000 people die every year in the U.S. due to accidental heart death. In certain cases, sudden cardiac death is caused by abnormally erratic heartbeats or tachycardia, which means that the heart cannot pump enough blood to the body.
Heart diseases are the most common cause of irregular heart rhythms. Often individuals are conscious of irregular heart rates, but sometimes they sense only their effects, such as fatigue or fainting. In Chaos, AIP Writing, researchers use mice to study tachycardia and found that there are underlying structures in cardiac tissue that they hypothesize contribute to the auto-determination of rapid cardiac rhythm.
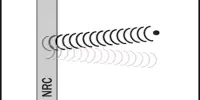
“A tachycardia is a heartbeat continuously activating the heart, like a toy train endlessly going around a circular track,” said co-author Leon Glass.
The heart is a muscular organ with four chambers built to operate effectively, consistently, and continuously over a lifespan. The muscular walls of each chamber contract in a regulated series, pumping blood as needed by the body and expending as little energy as possible with each heartbeat.

Controlling cardiac waves with light to better understand abnormally rapid heart rhythms
Researchers modeled tachycardia in the heart of the mouse by detecting the wave in one part of the heart and activating another part at a set time later. They observed that minor variations in the latency contribute either to infinite circulation or to the cardiac waves becoming self-contained. The heart rate is naturally controlled by the autonomic nervous system, which consists of the sympathetic and parasympathetic groups. Compassionate division raises the heart rhythm across a network of nerves called a sympathetic plexus.
During and before wave circulation, there was always an alternation of wave properties, such as one cycle proceeding faster and the next slower. The researchers used optogenetics, a set of instruments that enables them to induce and regulate cardiac waves with light rather than using traditional electrical stimulation techniques.
Arrhythmia is a cardiac condition where the heart beats abnormally. It is triggered by an electrical signal problem that coordinates the heartbeat. The heart will beat too rapidly, too slowly, or irregularly. In the past, alternating dynamics, called alternans, have been correlated in the heart with the initiation of tachycardia. As a result, attempts have been made to remove or limit alternates.
“Paradoxically, we find that alternans can also facilitate self-termination of tachycardia and might be beneficial,” said co-author Gil Bub.
An optical, real-time feedback control system can be used for a wide range of groundbreaking experiments beyond this particular study. “We could extend the work to study control of other geometries of abnormal cardiac wave propagation such as spiral waves. It can also be applied to the nervous system where there are abnormal bursting rhythms such as epilepsy,” said co-author Leonardo Sacconi.
The team plans to expand on this study in a variety of ways, including performing related studies in cardiac cell culture and exploring how drugs have an effect on tachycardia stabilization, characterizing molecular and ion pathways that promote tachycardia self-containment, and changing the magnitude of the alternators to examine their role in tachycardia self-containment.