One of the reasons cancer is so difficult to treat is the way it manipulates our immune system to work against us. Treatment kills some cancer cells, but what remains can “trick” our immune system into assisting tumor formation. A new study may have discovered a way to break this vicious circle.
Cancer cells migrate to other parts of the body through blood or lymphatic vessels when tumors spread. Scientists have discovered a new protein that prevents cancer cells from spreading by causing them to adhere more tightly to their surroundings. Their findings may one day aid doctors in determining the aggressiveness of a tumor and fine-tuning therapy.
It is unclear why some patients develop metastases while others do not. ISTA professor Daria Siekhaus and her colleagues are now contributing to a better understanding of the process in certain types of cancer. They investigated the role of a protein known as MFSD1 – a mammalian relative of a protein previously identified as affecting cell migration in fruit flies.
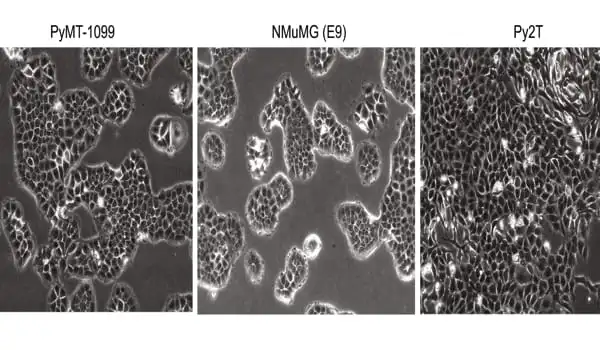
As a result, the Siekhaus group’s first author, Marko Roblek, created mouse cancer cells lacking the protein. Cells moved much faster without the protein, implying that MFSD1 keeps the cells from moving. The team tested their theory in living mice with breast, colon, and skin cancer in collaboration with collaborators from the University of Zurich.
“In the absence of MFSD1, there was a strong increase in metastasis,” Daria Siekhaus summarizes the results.
In the absence of MFSD1, there was a strong increase in metastasis. Apart from allowing the tumor to move more freely, we wanted to know why lower MFSD1 levels were beneficial to it. Cancer cells, for example, are subjected to a great deal of mechanical stress as they travel through the blood
Marko Roblek
Cancer cells resist starvation and stress
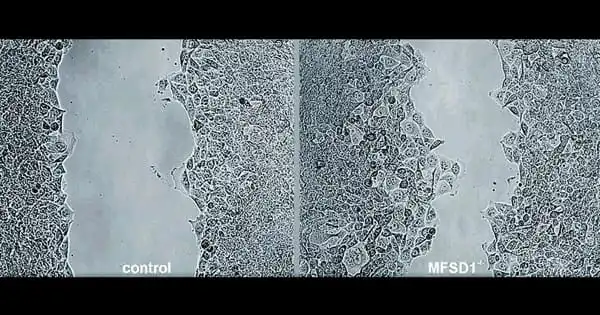
“Apart from allowing the tumor to move more freely, we wanted to know why lower MFSD1 levels were beneficial to it. Cancer cells, for example, are subjected to a great deal of mechanical stress as they travel through the blood” Marko Roblek elaborates. As a result, the researchers ran a stress test on cancer cells both with and without the protein. Roblek attempted to scrape the cells off the surface of the Petri dish in which he had grown them with a tiny rubber scraper.
While cancer cells containing MFSD1 died quickly when subjected to mechanical stress, those lacking the protein tended to survive. The team concluded that without the protein, certain tumor cells could more easily enter the bloodstream and spread to other parts of the body. A similar result was obtained when the researcher tested the cancer cell’s resistance to nutrient starvation in another experiment. Again, the cells lacking MFSD1 survived for a longer period of time.
Protein prevents detachment
The team was able to demonstrate that the protein MFSD1 is responsible for both the cell’s response to starvation and mechanical stress. It accomplishes this by influencing specific receptors on the cell’s surface. Integrins ensure that cells adhere to each other and to the extracellular matrix, a dense network that surrounds the cells in our bodies. The cell produces these receptors, transports them to the cell surface, and then transports them back inside the cell in a continuous circle. If a tumor cell lacks MFSD1, it is unable to recycle a specific type of integrin. “As a result, the cells stick less to the surrounding tissue and each other, making migration easier,” explains Daria Siekhaus.
Patient data supports findings
The team’s findings are also supported by Rita Seeböck of the University Hospital St. Pölten in Austria, who analyzed patient data. The data, which is available to researchers in anonymized form online, revealed a link between the level of MFSD1 and the patient’s prognosis. “We’ve seen that patients with specific types of breast, gastric, and lung cancer who had lower levels of MFSD1 had a worse outcome. A high level of MFSD1 appears to be protective; it acts as a suppressor of tumor metastasis “According to cancer researcher Roblek.
Doctors are already analyzing the expression of specific genes in order to optimize therapy for their patients. They can now look for the gene that codes for the protein MFSD1. “If this marker becomes more widely used, doctors will be able to use it to help classify how aggressive the cancer is and to choose between different treatment options,” says biologist Daria Siekhaus. In future studies, the researchers hope to learn more about how the protein works at the molecular level, as well as whether artificially increasing the amount of MFSD1 can help suppress the spread of certain tumors. The long-term goal is to investigate whether it can be used as a therapeutic target.