A basic eye test paired with strong artificial intelligence (AI) machine learning technologies could provide early detection of Parkinson’s disease, according to research presented at the annual meeting of the Radiological Society of North America (RSNA).
Parkinson’s disease is a progressive disorder of the central nervous system that affects millions of people worldwide. Diagnosis is typically based on symptoms like tremors, muscle stiffness, and impaired balance–an approach that has significant limitations. Making an accurate diagnosis of Parkinson’s disease can be complicated. Doctors must carefully weigh symptoms, family history, and other factors to come to a conclusion. Because there is no conclusive screening or test, patients with very early Parkinson’s disease may not meet the clinical diagnosis criteria.
Scientists have determined a simple eye exam combined with powerful artificial intelligence (AI) machine learning technology that could provide early detection of Parkinson’s disease.
“The issue with that method is that patients usually develop symptoms only after prolonged progression with a significant injury to dopamine brain neurons,” said study lead author Maximillian Diaz, a biomedical engineering Ph.D. student at the University of Florida in Gainesville, Florida. “This means that we are diagnosing patients late in the disease process.”
Work will be addressed at the annual conference of the Radiological Society of North America (RSNA). Parkinson’s disease is a chronic condition of the central nervous system that affects millions of people around the world. Diagnosis is usually based on signs such as tremors, muscle weakness, and poor balance—a method that has major drawbacks.
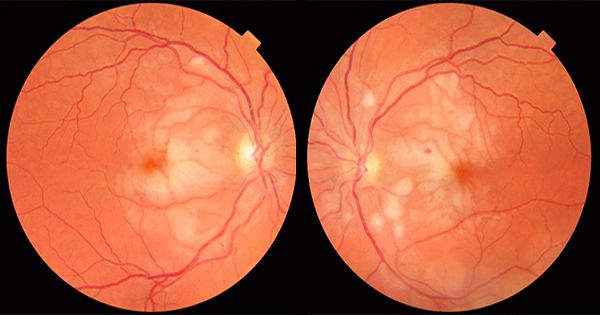
Progression of the condition is marked by a deterioration of the nerve cells that thins the walls of the retina, the sheet of tissue that forms the back of the eyeball. The condition also affects the retina’s small blood vessels or microvasculature. These characteristics offer an ability to use the strength of AI to analyze photographs of the eyes for symptoms of Parkinson’s disease.
Diaz has partnered with graduate student Jianqiao Tian and University of Florida neurologist Adolfo Ramirez-Zamora, M.D., under the leadership of Ruogu Fang, Ph.D., head of the J. Crayton Pruitt Department of Biomedical Engineering’s Smart Medical Informatics Learning and Assessment Center (SMILE).
Researchers have implemented a form of AI called support vector machine (SVM) learning that has been around since 1989. Using photographs of the back of the eye from both Parkinson’s disease patients and control subjects, SVM was learned to identify signs of disease in the pictures.
Results have shown that deep learning networks can classify Parkinson’s disease based on retinal vasculature, with the main features being smaller blood vessels. The suggested approaches further reinforce the theory that improvements in the physiology of the brain can be detected in the eye. “The single most significant discovery of this research was that a simple image of the eye was diagnosed with a brain disorder,” Diaz said. “It is really different from conventional approaches where to locate a brain issue you’re looking at different brain pictures.”
Diaz noted that these conventional imaging methods with MRI, CT and nuclear medicine methods can be very expensive. The new approach, on the other hand, uses basic photography with equipment commonly available in eye clinics to obtain an image. The photos can also be shot on a smartphone with a special lens.
“It’s just a clear image of the eye, you can do it in less than a minute, and the cost of the equipment is much less than a CT or MRI system,” Diaz said. “If we can do this on a regular basis, then the goal is that we can detect more patients faster, which can help us better understand the disease and find a treatment or a way to slow down the progression.”
The approach may also have applications in identifying other diseases that affect the structure of the brain, such as Alzheimer’s disease and multiple sclerosis, Diaz said.