Since the dawn of life on Earth, creatures have been both troubled and embraced by nanometer-sized intruders known as viruses, which seek refuge within the depths of cells. Although viruses frequently produce asymptomatic illnesses, some viruses have the ability to wreak havoc on populations in order to complete their infectious lifecycle.
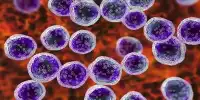
HIV infects a type of white blood cell called a T-helper cell, which is part of the body’s immune system (also called a CD4 cell). These critical cells keep us healthy by defending us against infections and disorders. HIV is incapable of reproducing on its own. Instead, the virus binds to and merges with a T-helper cell (joins together). It then takes over the cell’s DNA, replicates itself within the cell, and finally releases more HIV into the bloodstream. The HIV lifecycle refers to the process through which HIV multiplies and spreads throughout the body.
HIV affects the body’s natural defenses in this way, causing serious immune system damage over time. The virus develops at different rates depending on a person’s overall health, how quickly they are detected and begin antiretroviral treatment, and how regularly they take their medication.
When chronically HIV-1 infected people are put on effective antiretroviral medication therapy, the amount of virus in their blood diminishes, the viral reduction proceeded in two different phases, a quick first phase followed by a slow second phase.
Alan Perelson
A new study gives insight on the lifespans and locations of the cells responsible for HIV production, hindering its elimination. Understanding the behavior of the cells may aid scientists in developing novel methods to reduce their quantity, with the ultimate goal of treating HIV infection.
“When chronically HIV-1 infected people are put on effective antiretroviral medication therapy, the amount of virus in their blood diminishes,” stated Alan Perelson, Senior Fellow at Los Alamos National Laboratory. He and his colleague David D. Ho, MD, who is currently at Columbia University School of Medicine, discovered that “the viral reduction proceeded in two different phases, a quick first phase followed by a slow second phase.”
Using Perelson’s mathematical model of viral infection and treatment, the team determined that the two-phase drop was due to HIV infecting two separate cell populations that produced HIV. The majority of the virus was produced by one population, although it only lived for a day or two. According to the model, the first phase drop of the virus in the blood was caused by the degradation of this population.

The second cell population, which generated virus at a slower rate, lived for a few weeks while producing virus, and their demise was responsible for the second phase of viral degradation detected in the blood, according to the study.
Now, in a new paper published this week in the journal PNAS, Robert Siliciano, MD, of Johns Hopkins University School of Medicine and his team, in collaboration with Perelson and Ruy Ribeiro of the Theoretical Biology and Biophysics Group at Los Alamos National Laboratory, searched for these hypothesized cells with different decay rates. Siliciano’s team isolated HIV-infected cells in the blood of 17 persons living with HIV who were on antiretroviral therapy twice a month for the first three months, and subsequently once a month for a year.
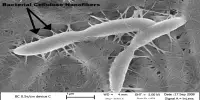
They discovered that only few of the short-lived infected cells responsible for the first phase of viral decay were circulating in the circulation, implying that these cells are most likely present in tissues like lymph nodes and the spleen.
Instead, they discovered in the blood cells with an entire HIV genome that degraded with a half-life of roughly two weeks. These are the cells that, according to Perelson and Ho, are responsible for the second phase of viral disintegration. After three months of treatment, the remaining infected cells with intact HIV genomes degraded even more slowly, with a half-life of roughly 19 months. These cells may become part of the latent-infected cell reservoir, which if therapy is stopped re-seeds the infection and virus then becomes detectable usually in a matter of weeks.
Antiretroviral therapy for HIV combines a variety of medications, each of which targets a different stage of the HIV lifecycle. This means that HIV replication is halted on numerous fronts, making it extremely effective. If taken properly, it strengthens the immune system, prevents the signs and illnesses associated with AIDS from developing, and allows people to live long and healthy lives.
If a person does not take their medication appropriately or regularly (at the same time every day), the amount of HIV in their blood may rise and the treatments may no longer be effective. This is referred to as drug resistance.